CALL TODAY 646-846-1136 | EMAIL
Surgical Experts Dedicated to Improving Lives
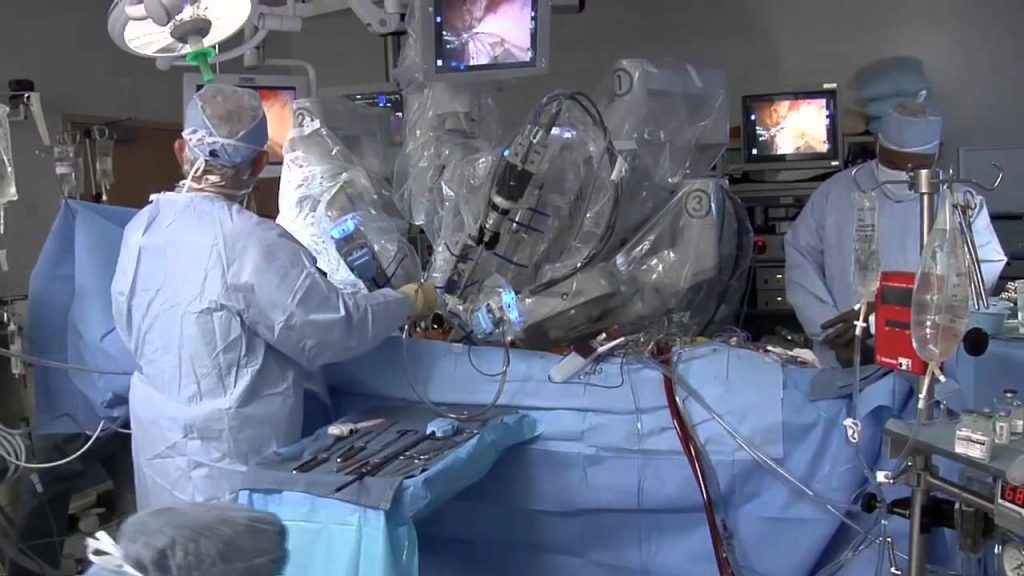
At Lenox Hill Surgeons, our dedicated team of nyc surgeons and medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments.We specialize in general surgery, including extensive experience in performing hernia repair surgery. Our expertise is in minimally invasive surgery and robotic surgery. Minimally invasive and robotic surgery often allow patients to experience easier recovery than traditional open surgery. They also allow for more precise and less traumatic surgery. When robotic and minimally invasive surgery is not an option, we are also skilled and experienced in traditional open surgical procedures.
All of our doctors are experienced and skilled surgeons having undergone extensive training in school, residency and fellowships. They all practice medicine with ethical behavior, compassion and superb bedside manner. In the operating room they all exhibit precise mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These innate and learned skills allow our surgeons to be some of the most dexterous and skilled professionals in all of New York City and the Country.
Call us: 646-846-1136
About The Surgeons
PATIENT TESTIMONIALS
Recent Awards
We are honored and deeply appreciative to have consistently received prestigious awards and recognition year after year, establishing us as one of New York’s foremost hospitals for a wide range of general surgeries, safety measures, specialized procedures, and overall excellence in healthcare. At Lenox Hill Surgeons, our unwavering commitment lies in delivering exceptional care and unwavering support to our patients, guaranteeing their safety and successful recovery throughout their entire surgical experience.
Hospital Quality Awards
 America’s 50 Best Hospitals Award™ (2023, 2022)
America’s 50 Best Hospitals Award™ (2023, 2022)
Top 1% in the nation for providing the highest clinical quality year over year.

America’s 100 Best Hospitals Award™ (2021)
Top 2% in the nation for consistently delivering clinical quality year over year.

America’s 250 Best Hospitals Award™ (2023, 2022, 2021)
Top 5% in the nation for consistently delivering clinical quality.

Patient Safety Excellence Award™ (2023, 2022)
Top in the nation for providing excellence in patient safety by preventing infections, medical errors, and other preventable complications.
Specialty Clinical Quality Awards

America’s 100 Best Hospitals for Cardiac Care Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in heart bypass surgery, coronary interventional procedures, heart attack treatment, heart failure treatment, and heart valve surgery.

America’s 100 Best Hospitals for Coronary Intervention Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in coronary intervention procedures (angioplasty with stent).

America’s 100 Best Hospitals for Prostate Surgery Award™ (2023, 2022, 2021)
Superior clinical outcomes in prostate removal surgery and transurethral resection of the prostate.
Click to see all of our Healthgrades best doctors awards


Visit our main website at www.LenoxHillSurgeons.com
Blog Posts are Below:
Hernia Repair Surgery – NYC Surgeon
Hernia Repair Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
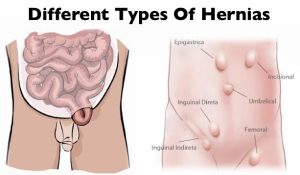 Hernia repair surgery entails the application of instrumental and manual procedures for correcting herniation of tissues or viscera including groin, abdomen, brain, and diaphragm. Internal organs, composed of tissues, could get herniated or bulged, forcing them to protrude via the wall encasing them. Hernias involving the groin (an inguinal hernia) and the umbilical cord (an umbilical hernia) are two of the most prevalent forms of a hernia.
Hernia repair surgery entails the application of instrumental and manual procedures for correcting herniation of tissues or viscera including groin, abdomen, brain, and diaphragm. Internal organs, composed of tissues, could get herniated or bulged, forcing them to protrude via the wall encasing them. Hernias involving the groin (an inguinal hernia) and the umbilical cord (an umbilical hernia) are two of the most prevalent forms of a hernia.
Since a hernia does not heal on its own but rather expands over time, it is crucial that you opt for surgical treatment to avoid unnecessary/preventable complications in the long run. Hernia surgery, usually performed on an outpatient basis, is a moderately simple operation that can help remedy the organ’s bulging and restore it to its original position.
Steps
 Two of the most popular types of hernia repair surgery is ‘herniorrhaphy’ and ‘hernioplasty’. Herniorrhaphy-the traditional hernia repair technique-is still conducted extensively where the surgeon makes a wide and long notch over the herniated organ. Thereafter, the physician removes the protrusion and reinstates the dislodged organ or tissues to its actual site.
Two of the most popular types of hernia repair surgery is ‘herniorrhaphy’ and ‘hernioplasty’. Herniorrhaphy-the traditional hernia repair technique-is still conducted extensively where the surgeon makes a wide and long notch over the herniated organ. Thereafter, the physician removes the protrusion and reinstates the dislodged organ or tissues to its actual site.
Finally, the doctor sutures the hole in the muscle via which the protuberance developed, sterilizes the incision, and sews it up. Hernioplasty is very much similar to herniorrhaphy procedurally excepting that in the final step, the surgeon overlays a sterile mesh (produced from animal tissues or polypropylene) on the muscular notch rather than suturing it. The nature or type of your herniation will determine the mode of repair surgery you’ll need to opt for.
Strangulated, reducible, and irreducible hernias are the three most widespread kinds of hernias. Both of the aforementioned surgical operation procedures can be carried out using a laparoscope or via open surgery.
Benefits
Both hernioplasty and herniorrhaphy are straightforward and uncomplicated surgical repair processes that take about 30-40 minutes to complete. You won’t feel any pain as the surgery will be done using either local or general anesthesia. Majority of patients are discharged from the hospital or medical center on the very day the laparoscopic surgery is performed. The usual benefits of the laparoscopic repair operation include:-
- Very short duration of stay
- Faster healing
- Reduced pain post surgery
- Quicker return to normal life
- Minimal costs (including all the expense heads)
- Lower risks of infection
Side Effects
The side effects of this type of surgery, most of which are rare, involve:-
- Swelling and redness around the incision or opening
- Blood clot
- Mesh pain
- Urinary tract infection
- Urinary incontinence
- Infection
- Difficulty urinating
- Hernia recurrence
- Neuralgia or nerve damage
- Constipation
- Kidney failure or complications
- Breathing problems or pneumonia
Precautions
You must abide by the surgeon’s instructions once you return home (which are usually on the same day the surgery is carried out) for a speedy recovery. Take all the prescribed medications on time, including the anti-inflammatory drugs for minimizing the possibilities of incision swelling. Contact your surgeon instantly if you’ve recurrent spells of fever, coughs, chills, nausea, abdominal swelling, bleeding as well as experience difficulty in urinating. Make sure you get sufficient rest for at least two weeks following the operation so that you can get back to work at the earliest.
Prognosis
Most hernia surgeries are effective, enabling patients to recover fully within 4-6 weeks. A typical person who has undergone hernia repair surgery can resume normal activities 2 weeks after the procedure.
Concluding Remarks
Opting for a surgical procedure for remedying a hernia is highly recommended not only for avoiding complications which could take a fatal turn (though very rare) but also for going back to leading a normal life. You can make an appointment with our general surgeon for a detailed, one-to-one consultation.
References
- http://www.medtronic.com/us-en/patients/treatments-therapies/hernia-surgery/about-recovery.html
- https://www.webmd.com/digestive-disorders/inguinal-hernia#1
- https://www.medicalnewstoday.com/articles/319753.php
- https://www.highgatehospital.co.uk/things-you-need-to-know-hernia-operation/
- https://www.webmd.com/digestive-disorders/need-surgery-hernia#1
- http://columbiasurgery.org/news/2014/04/15/hernias-what-you-need-know
- https://en.wikipedia.org/wiki/Hernia_repair
- https://my.clevelandclinic.org/health/treatments/6905-laparoscopic-surgery-for-hernia-repair/risks–benefits
General Surgery
Here are some brief descriptions about the different types of general surgery we perform:
Laparoscopic surgery
This is a relatively new specialty dealing with minimal access techniques using cameras and small instruments inserted through 0.3 to 1 cm incisions. Robotic surgery is now evolving from this concept (see below). Gallbladders, appendices, and colons can all be removed with this technique. Hernias are now repaired mostly laparoscopically. Most bariatric surgery is performed laparoscopically.[citation needed] General surgeons that are trained today are expected to be proficient in laparoscopic procedures.
Colorectal surgery
General surgeons treat a wide variety of major and minor colon and rectal diseases including inflammatory bowel diseases (such as ulcerative colitis or Crohn’s disease), diverticulitis, colon and rectal cancer, gastrointestinal bleeding and hemorrhoids.
Endocrine surgery
General surgeons are trained to remove all or part of the thyroid and parathyroid glands in the neck and the adrenal glands just above each kidney in the abdomen. In many communities, they are the only surgeon trained to do this. In communities that have a number of subspecialists, other subspecialty surgeons may assume responsibility for these procedures.
Surgical oncology
Surgical oncologist refers to a general surgical oncologist (a specialty of a general surgeon), but thoracic surgical oncologists, gynecologist and so forth can all be considered surgeons who specialize in treating cancer patients. The importance of training surgeons who sub-specialize in cancer surgery lies in evidence, supported by a number of clinical trials, that outcomes in surgical cancer care are positively associated to surgeon volume—i.e., the more cancer cases a surgeon treats, the more proficient he or she becomes, and his or her patients experience improved survival rates as a result. This is another controversial point, but it is generally accepted—even as common sense—that a surgeon who performs a given operation more often, will achieve superior results when compared with a surgeon who rarely performs the same procedure. This is particularly true of complex cancer resections such as pancreaticoduodenectomy for pancreatic cancer, and gastrectomy with extended (D2) lymphadenectomy for gastric cancer. Surgical oncology is generally a 2 year fellowship following completion of a general surgery residency (5-7 years).
Contact us at 646-846-1136 to schedule an appointment.
Patient Testimonials for Lenox Hill Surgeons
Liver Surgery: Procedures for Liver Diseases and Tumors
In this article, we will explore common liver conditions, their symptoms, and the surgical procedures for liver diseases and tumors. The liver is a vital organ responsible for numerous functions, including detoxification, metabolism, and the production of essential proteins. However, various conditions can affect the liver, ranging from benign liver cysts to liver tumors. When conservative treatments fail to provide relief or when liver tumors require intervention, liver surgery may be necessary. At Lenox Hill Surgeons, a trusted general surgery practice in New York City, our expert surgeons specialize in liver surgery, offering advanced procedures for liver diseases and tumors.

Common Liver Diseases and Tumors
The liver can be affected by a range of diseases and tumors, including:
1. Hepatitis:
Hepatitis is an inflammation of the liver often caused by viral infections, such as hepatitis A, B, or C. Chronic hepatitis can lead to liver damage and the development of liver diseases.
2. Liver Cirrhosis:
Liver cirrhosis is a progressive scarring of the liver due to long-term damage, typically caused by chronic hepatitis, alcohol abuse, or certain metabolic diseases. Cirrhosis can impair liver function and lead to complications.
3. Liver Cysts:
Liver cysts are fluid-filled sacs that can develop within the liver. Most liver cysts are benign and do not require treatment. However, large or symptomatic cysts may require surgical intervention.
4. Liver Tumors:
Liver tumors can be either benign (non-cancerous) or malignant (cancerous). Benign liver tumors, such as hemangiomas or adenomas, may require surgical removal if they cause symptoms or pose a risk. Malignant liver tumors, such as hepatocellular carcinoma or metastatic tumors, often necessitate surgical treatment, along with other therapies.
Surgical Procedures for Liver Diseases and Tumors
Liver surgery encompasses various procedures, depending on the specific condition and its severity. Some common surgical interventions for liver diseases and tumors include:
1. Liver Resection:
Liver resection involves the surgical removal of a portion of the liver affected by tumors or diseases. This procedure aims to remove the diseased or cancerous tissue while preserving sufficient healthy liver tissue.
2. Liver Transplantation:
Liver transplantation is performed in cases of end-stage liver disease or advanced liver cancer. It involves replacing the diseased liver with a healthy liver from a deceased or living donor.
3. Ablation Therapy:
Ablation therapy utilizes techniques such as radiofrequency ablation, microwave ablation, or cryoablation to destroy tumors within the liver. These minimally invasive procedures can be effective for small liver tumors.
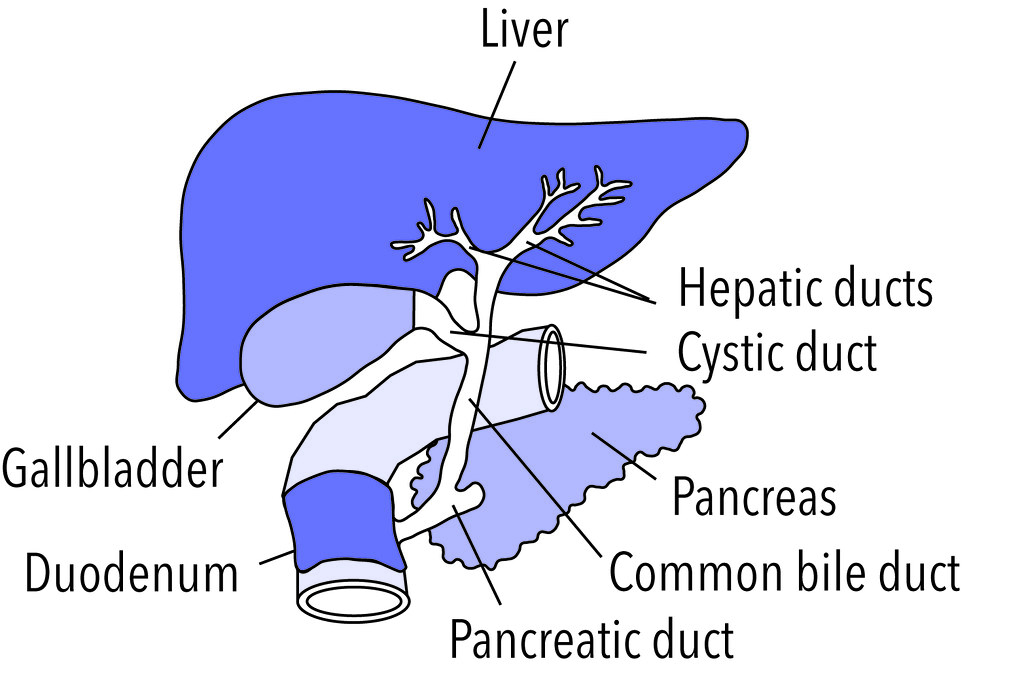
4. Biliary Surgery:
Biliary surgery addresses conditions affecting the bile ducts, which carry bile from the liver to the small intestine. Procedures such as bile duct repair, bile duct resection, or the creation of biliary bypasses may be necessary to restore proper bile flow.
Expert Liver Surgery Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we understand the complexity of liver diseases and tumors, and our skilled team of surgeons is committed to providing the highest level of care. We utilize advanced surgical techniques and individualized treatment plans to ensure optimal outcomes for our patients.
Contact us today to schedule a consultation and benefit from the expertise of our renowned surgeons.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Robotic Assisted General Surgery: Advancements in Manhattan
In this comprehensive article, we will explore the benefits of robotic assisted general surgery and how it is transforming the landscape of surgical procedures. Advancements in surgical technology have revolutionized the field of general surgery, providing surgeons with innovative tools and techniques to deliver improved outcomes for patients. One such advancement is robotic-assisted surgery, which has gained popularity in recent years. At Lenox Hill Surgeons, a renowned general surgery practice in Manhattan, we embrace cutting-edge technologies, including robotic-assisted surgery, to offer our patients the highest level of surgical care.

What is Robotic Assisted General Surgery?
Robotic assisted general surgery involves the use of robotic technology to assist surgeons during surgical procedures. It combines the precision and dexterity of robotic systems with the expertise of the surgeon, allowing for enhanced visualization, greater control, and improved surgical outcomes. The da Vinci Surgical System is one of the most widely used robotic systems in general surgery, enabling surgeons to perform complex procedures with enhanced accuracy and efficiency.
The Benefits of Robotic Assisted General Surgery
Robotic assisted general surgery offers several advantages over traditional open surgery and even laparoscopic surgery:
1. Enhanced Precision:
Robotic systems provide high-definition, magnified 3D visualization of the surgical site. This level of precision allows surgeons to navigate intricate anatomical structures with improved accuracy, reducing the risk of damage to surrounding tissues.
2. Greater Dexterity:
Robotic assisted surgery offers increased range of motion and flexibility compared to human hands alone. The robotic arms can rotate 360 degrees and perform complex maneuvers with precision, enabling surgeons to access hard-to-reach areas more easily.
3. Reduced Trauma:
The minimally invasive nature of robotic-assisted surgery results in smaller incisions, leading to less tissue trauma, reduced post-operative pain, and minimal scarring. Patients often experience faster recovery times and a shorter hospital stay.
4. Improved Visualization:
The high-definition 3D visualization provided by robotic systems allows surgeons to see intricate details of the surgical site more clearly. This enhances their ability to identify and address potential complications, leading to improved surgical outcomes.
5. Increased Safety:
Robotic systems incorporate advanced technologies, such as real-time imaging and motion scaling, that enhance patient safety during surgery. Surgeons can precisely control movements, reducing the risk of accidental tissue damage.
Robotic Assisted Procedures in General Surgery
Robotic-assisted surgery is utilized in various general surgical procedures. Some common examples include:
1. Hernia Repair:
Robotic technology allows surgeons to repair different types of hernias with improved precision and control. The robotic system assists in mesh placement, suture placement, and other complex maneuvers required during hernia repair surgery.
2. Gallbladder Surgery:
Robotic assisted techniques offer enhanced visualization and dexterity for gallbladder removal surgery. Surgeons can perform cholecystectomy with smaller incisions, reducing post-operative pain and scarring.
3. Colorectal Surgery:
Robotic systems enable surgeons to perform intricate colorectal procedures, such as rectal resection and colon resection, with enhanced precision and control. This approach may result in faster recovery and better functional outcomes for patients.
4. Bariatric Surgery:
Robotic technology plays a valuable role in bariatric surgery, providing surgeons with the necessary tools to perform gastric bypass or sleeve gastrectomy procedures. The robotic system facilitates precise suturing and stapling, contributing to optimal surgical outcomes.
Expert Robotic Assisted Surgery Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we are at the forefront of surgical advancements and embrace robotic assisted surgery as part of our commitment to delivering exceptional care. Our team of experienced surgeons is highly skilled in utilizing robotic technology to perform a wide range of general surgical procedures. We prioritize patient safety, personalized treatment plans, and compassionate care throughout the surgical journey.
Contact us today to schedule a consultation with our surgeons.
Contact Information:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Adrenal Gland Disorders: Surgical Approaches and Treatment Considerations
 In this informative article, we will explore common adrenal gland disorders, their symptoms, and the surgical treatment options available. The adrenal glands, located on top of each kidney, are responsible for producing essential hormones that regulate various bodily functions. However, certain conditions can disrupt the normal functioning of the adrenal glands, leading to adrenal gland disorders. While non-surgical treatments are often effective, surgical intervention may be necessary in some cases. At Lenox Hill Surgeons, a trusted general surgery practice in New York City, our expert surgeons specialize in adrenal gland disorders and provide advanced surgical approaches to address these conditions.
In this informative article, we will explore common adrenal gland disorders, their symptoms, and the surgical treatment options available. The adrenal glands, located on top of each kidney, are responsible for producing essential hormones that regulate various bodily functions. However, certain conditions can disrupt the normal functioning of the adrenal glands, leading to adrenal gland disorders. While non-surgical treatments are often effective, surgical intervention may be necessary in some cases. At Lenox Hill Surgeons, a trusted general surgery practice in New York City, our expert surgeons specialize in adrenal gland disorders and provide advanced surgical approaches to address these conditions.
Common Adrenal Gland Disorders
The adrenal glands can be affected by different disorders, including:
1. Adrenal Tumors:
Adrenal tumors are abnormal growths that can be benign (non-cancerous) or malignant (cancerous). These tumors can overproduce hormones, leading to hormonal imbalances and various symptoms.
2. Cushing’s Syndrome:
Cushing’s syndrome occurs when the adrenal glands produce excessive amounts of cortisol, a hormone that regulates metabolism. Symptoms may include weight gain, high blood pressure, and muscle weakness.
3. Conn’s Syndrome:
Conn’s syndrome, also known as primary hyperaldosteronism, occurs when the adrenal glands produce too much aldosterone. This hormone regulates sodium and potassium levels, and an excess can lead to high blood pressure and electrolyte imbalances.
4. Pheochromocytoma:
A pheochromocytoma is a rare tumor that develops in the adrenal glands. It causes the glands to produce excessive amounts of adrenaline and noradrenaline, resulting in episodes of high blood pressure, rapid heartbeat, and sweating.
Surgical Approaches to Adrenal Gland Disorders
When non-surgical treatments are ineffective or the adrenal gland disorder poses a significant risk to the patient’s health, surgical intervention may be recommended. The most common surgical approach for adrenal gland disorders is adrenalectomy, which involves the removal of the affected adrenal gland(s). There are two main types of adrenalectomy:
1. Open Adrenalectomy:
Open adrenalectomy is a traditional surgical approach that involves making a larger incision to access and remove the affected adrenal gland(s). This approach may be necessary for larger tumors or complex cases.
2. Laparoscopic Adrenalectomy:
Laparoscopic adrenalectomy is a minimally invasive procedure that utilizes small incisions and specialized instruments. A laparoscope, a thin tube with a camera, is inserted through one of the incisions to visualize the surgical area. The surgeon then removes the adrenal gland(s) using precise instruments inserted through the other small incisions. Laparoscopic adrenalectomy offers advantages such as reduced post-operative pain, shorter hospital stays, and faster recovery compared to open surgery.
Expert Surgical Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we understand the complexities of adrenal gland disorders and the importance of personalized care. Our team of experienced general surgeons specializes in adrenal gland surgeries, utilizing advanced techniques to ensure optimal outcomes for our patients. We are dedicated to providing comprehensive evaluations, individualized treatment plans, and compassionate care throughout your surgery.
Contact us today to schedule a consultation with our renowned surgeons.
Contact Information:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Preparing for General Surgery: A Step-by-Step Guide
In this step-by-step guide, we will walk you through the key aspects of preparing for general surgery to help you feel confident and informed. Facing the prospect of general surgery can be daunting, but proper preparation can help alleviate anxiety and ensure a smoother recovery process. Whether you’re scheduled for a routine procedure or a more complex surgical intervention, being well-prepared is essential. At Lenox Hill Surgeons, a trusted general surgery practice in New York City, we believe in providing comprehensive care to our patients.

Preparing for General Surgery: A Step-by-Step Guide
Step 1: Consultation and Preoperative Evaluation
The first step in preparing for general surgery is scheduling a consultation with your surgeon. During this appointment, your surgeon will review your medical history, perform a physical examination, and discuss the details of your upcoming surgery. This is also an opportunity to address any questions or concerns you may have. Your surgeon may order preoperative tests, such as bloodwork or imaging, to ensure you are in optimal condition for surgery.
Step 2: Preoperative Instructions
Your surgeon and their team will provide you with specific preoperative instructions tailored to your procedure. These instructions may include dietary restrictions, medication guidelines, and guidance on preparing your body for surgery. It is crucial to follow these instructions carefully to minimize potential complications and ensure the best possible outcome.
Step 3: Lifestyle Adjustments
Depending on your procedure, you may need to make certain lifestyle adjustments in the days or weeks leading up to surgery. This may involve quitting smoking, avoiding certain medications or supplements that can interfere with the surgery, and adjusting your diet to promote healing. Your surgeon will provide guidance on these adjustments based on your individual needs.
Step 4: Preparing Your Support System
Having a strong support system is invaluable during the surgical process. Arrange for someone to accompany you to the hospital on the day of surgery and stay with you during the initial recovery period. This person can provide emotional support, help with practical matters, and assist you in following postoperative instructions.
Step 5: Mental and Emotional Preparation
Surgery can be emotionally challenging, so it’s important to take care of your mental well-being. Engage in relaxation techniques, such as deep breathing exercises or meditation, to help manage stress and anxiety. Stay informed about your procedure but avoid excessive online research that may increase worry. Trust in the expertise of your surgeon and the healthcare team supporting you.
Step 6: Preparing for Hospital Stay
If your surgery requires an overnight hospital stay, pack a small bag with essential items, such as comfortable clothing, toiletries, and any necessary medications. Follow fasting instructions provided by your surgeon to ensure your stomach is empty before the procedure. Arrive at the hospital on time, and be prepared for necessary paperwork and preoperative preparations.
Step 7: Postoperative Recovery Plan
Before your surgery, discuss the postoperative recovery plan with your surgeon. Understand what to expect in terms of pain management, wound care, dietary guidelines, and activity restrictions. Arrange for follow-up appointments and ensure you have the necessary support and resources in place for a smooth recovery at home.
Expert General Surgical Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we are dedicated to providing exceptional surgical care and support throughout your surgical journey. Our team of experienced general surgeons utilizes advanced techniques and compassionate care to ensure optimal outcomes and patient satisfaction.
Contact us today to schedule a consultation and benefit from the expertise of our renowned surgeons.
Contact Information:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
https://lenoxhillsurgeons.com/
Gallbladder Surgery: Common Disorders and Surgical Solutions
Various conditions can affect the gallbladder, leading to discomfort and potential complications. Gallbladder surgery may be necessary when conservative treatments fail to alleviate symptoms. The gallbladder is a small organ located beneath the liver that plays a vital role in the digestion of fats. At Lenox Hill Surgeons, a leading general surgery practice in New York City, our team of expert surgeons specializes in gallbladder surgery, offering patients effective surgical solutions for gallbladder disorders. In this comprehensive article, we will explore common gallbladder disorders, their symptoms, and the surgical interventions available to provide relief and restore well-being.
Gallstones: Causes and Symptoms
Gallstones are one of the most common disorders affecting the gallbladder. They are formed when substances in bile, such as cholesterol or bilirubin, harden into stone-like particles. Gallstones can range in size and quantity, and they can cause various symptoms, including:
1. Abdominal Pain:
Gallstones often cause intense pain in the upper right abdomen or in the middle of the abdomen just below the breastbone. The pain can be recurrent and may radiate to the back or shoulder.
2. Nausea and Vomiting:
Gallstone-related pain can lead to feelings of nausea and sometimes result in vomiting.
3. Jaundice:
In some cases, gallstones can obstruct the bile duct, leading to a buildup of bilirubin in the body. This can cause yellowing of the skin and eyes, known as jaundice.
4. Indigestion and Bloating:
Gallstones can disrupt the normal flow of bile, leading to indigestion, bloating, and a feeling of fullness after meals.

Gallbladder Surgery: Cholecystectomy
When gallstones or other gallbladder disorders cause significant symptoms or complications, gallbladder surgery is often recommended. The most common surgical intervention for gallbladder removal is called cholecystectomy. There are two primary approaches to cholecystectomy:
1. Laparoscopic Cholecystectomy:
Laparoscopic cholecystectomy is a minimally invasive surgical procedure that utilizes small incisions and specialized instruments. The surgeon inserts a laparoscope, a thin tube with a camera, to visualize the surgical area. The gallbladder is then removed through small incisions, resulting in less post-operative pain, faster recovery, and minimal scarring.
2. Open Cholecystectomy:
Open cholecystectomy is a traditional surgical approach that involves making a larger incision in the abdomen to remove the gallbladder. While it requires a larger incision and longer recovery time compared to laparoscopic cholecystectomy, open cholecystectomy may be necessary in certain cases, such as when there are complications or if laparoscopic surgery is not feasible.
Expert Gallbladder Surgery Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we understand the impact gallbladder disorders can have on your daily life. Our team of experienced general surgeons specializes in gallbladder surgery and provides individualized care to meet your specific needs. We utilize advanced techniques and state-of-the-art technology to ensure optimal surgical outcomes and patient satisfaction.
Contact us today to schedule a consultation and benefit from the expertise of our renowned surgeons:
Contact Information:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
https://lenoxhillsurgeons.com/
Common General Surgeries and Their Importance for Patients
When it comes to addressing various health conditions and improving quality of life, general surgery plays a crucial role. General surgeons are skilled professionals who specialize in a wide range of surgical procedures. At Lenox Hill Surgeons, a renowned general surgery practice in New York City, our team of expert surgeons is dedicated to providing exceptional care and expertise. In this informative article, we will explore some common general surgeries and their importance in helping patients regain their health and well-being.

Hernia Repair: Restoring Comfort and Functionality
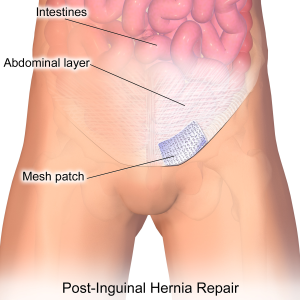 Hernias occur when an organ or tissue protrudes through a weakened area in the surrounding muscle or connective tissue. Hernia repair is a common general surgery procedure that aims to correct this condition. Whether it’s an inguinal hernia in the groin area or an umbilical hernia near the navel, hernia repair surgery helps restore comfort and functionality to patients. By repairing the weakened area and reinforcing it with sutures or a mesh patch, general surgeons provide a long-term solution for hernia patients.
Hernias occur when an organ or tissue protrudes through a weakened area in the surrounding muscle or connective tissue. Hernia repair is a common general surgery procedure that aims to correct this condition. Whether it’s an inguinal hernia in the groin area or an umbilical hernia near the navel, hernia repair surgery helps restore comfort and functionality to patients. By repairing the weakened area and reinforcing it with sutures or a mesh patch, general surgeons provide a long-term solution for hernia patients.
Appendix Surgery: Preventing Complications
Appendicitis is a condition characterized by inflammation of the appendix. If left untreated, a ruptured appendix can lead to severe complications and even be life-threatening. Appendix surgery, also known as an appendectomy, is a common surgical intervention that involves the removal of the inflamed appendix. General surgeons perform this procedure promptly to prevent the risk of complications and ensure a complete recovery for patients.
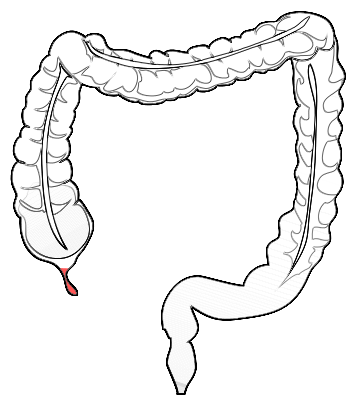
Colon Surgery: Treating Colon Conditions
Colon surgery addresses various conditions affecting the large intestine, such as colon cancer, diverticulitis, and inflammatory bowel disease. General surgeons specializing in colon surgery utilize advanced techniques, such as laparoscopic or robotic-assisted surgery, to remove diseased portions of the colon and restore normal bowel function. Early detection and timely intervention through colon surgery are essential in improving patient outcomes and ensuring long-term well-being.
Gallbladder Surgery: Alleviating Gallbladder Disorders
Gallbladder surgery, known as cholecystectomy, is performed to treat gallbladder-related conditions, such as gallstones or inflammation. General surgeons employ both traditional open surgery and minimally invasive laparoscopic techniques to remove the gallbladder. Gallbladder surgery not only alleviates pain and discomfort but also prevents the recurrence of gallstones and potential complications, allowing patients to resume their normal lives.
Thyroid Surgery: Managing Thyroid Disorders
Thyroid surgery is performed to address thyroid disorders, such as thyroid nodules, goiters, or thyroid cancer. General surgeons skilled in thyroid surgery aim to remove all or part of the thyroid gland, depending on the specific condition. By managing thyroid disorders through surgery, general surgeons help restore hormonal balance and prevent the progression of thyroid-related complications, ensuring patients’ overall well-being.
Common General Surgeries: Receive Expert General Surgical Services at Lenox Hill Surgeons in New York
At Lenox Hill Surgeons, we understand the importance of common general surgeries in addressing various health conditions. Our team of experienced general surgeons are committed to delivering exceptional surgical care, utilizing advanced techniques, and prioritizing patient well-being. If you require any general surgical services, trust our expertise and experience for outstanding outcomes.
Contact us today to schedule a consultation and benefit from the expertise of our renowned surgeons:
Contact Information:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Understanding Laparoscopic Surgery: Minimally Invasive Procedures in Manhattan
In this informative article, we will explore laparoscopic surgery, its advantages, and the range of procedures it encompasses. Advancements in surgical techniques have revolutionized the field of medicine, allowing for more precise and minimally invasive procedures. Laparoscopic surgery, also known as keyhole surgery, has gained popularity for its numerous benefits compared to traditional open surgery. Lenox Hill Surgeons, a leading general surgery practice in Manhattan, specializes in this type of surgery, offering patients advanced and minimally invasive treatment options.

What is Laparoscopic Surgery?
Laparoscopic surgery is a minimally invasive surgical technique that utilizes small incisions and specialized surgical instruments. It involves the use of a laparoscope, a thin tube with a camera and light source, which allows the surgeon to visualize the surgical area in high definition. The images captured by the laparoscope are projected onto a monitor, guiding the surgeon throughout the procedure.
The Advantages of Laparoscopic Surgery
Laparoscopic surgery offers several advantages over traditional open surgery:
1. Minimally Invasive:
The use of small incisions results in less tissue trauma, leading to reduced post-operative pain, less scarring, and faster recovery times compared to open surgery.
2. Reduced Blood Loss:
Laparoscopic procedures involve precise incisions and the use of specialized instruments, which help minimize blood loss during surgery.
3. Enhanced Visualization:
The laparoscope provides a magnified and detailed view of the surgical site, allowing surgeons to perform intricate procedures with improved precision.
4. Shorter Hospital Stay:
Laparoscopic surgery often allows for shorter hospital stays, enabling patients to return to their daily activities and routines more quickly.
5. Quicker Recovery:
With reduced post-operative pain and smaller incisions, patients experience faster recovery times, allowing them to resume their regular activities sooner.
Common Laparoscopic Procedures
Laparoscopic surgery is employed in various general surgical procedures. Here are some common examples:
1. Laparoscopic Cholecystectomy:
This procedure involves the removal of the gallbladder through small incisions. Laparoscopic cholecystectomy is a highly effective treatment for gallstones and gallbladder disease.
2. Laparoscopic Appendectomy:
Appendectomy is the surgical removal of the appendix. Laparoscopic appendectomy is the preferred approach for most cases of appendicitis, resulting in less pain, faster recovery, and minimal scarring.
3. Laparoscopic Hernia Repair:
Laparoscopic techniques are commonly used to repair different types of hernias, such as inguinal, femoral, or umbilical hernias. This approach provides excellent results with minimal post-operative discomfort.
4. Laparoscopic Colon Resection:
Laparoscopic colon resection involves the removal of a portion of the colon affected by conditions such as colon cancer, diverticulitis, or inflammatory bowel disease. It offers benefits such as reduced pain and faster recovery.
Expert Laparoscopic Surgery Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we understand the importance of advanced surgical techniques in improving patient outcomes and quality of life. Our skilled team of general surgeons specializes in laparoscopic surgery, utilizing the latest technologies and techniques to ensure the best results for our patients.
Contact us today to schedule a consultation and benefit from the expertise of our renowned surgeons:
Contact Information:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Appendix Surgery: Understanding Appendicitis and Surgical Interventions
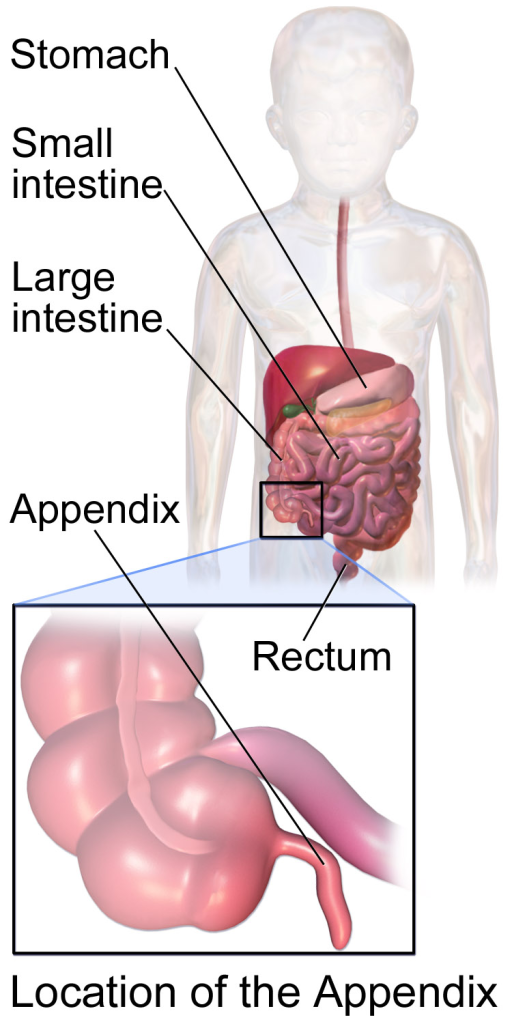 In this informative article, we will explore appendicitis, its symptoms, and the surgical interventions available for its treatment. The appendix may be a small organ in the human body, but when it becomes inflamed, it can cause significant pain and discomfort. Appendicitis is a common condition that often requires surgical intervention to prevent complications. At Lenox Hill Surgeons, a leading general surgery practice in New York City, our skilled surgeons specialize in appendix surgery.
In this informative article, we will explore appendicitis, its symptoms, and the surgical interventions available for its treatment. The appendix may be a small organ in the human body, but when it becomes inflamed, it can cause significant pain and discomfort. Appendicitis is a common condition that often requires surgical intervention to prevent complications. At Lenox Hill Surgeons, a leading general surgery practice in New York City, our skilled surgeons specialize in appendix surgery.
Understanding Appendicitis
Appendicitis occurs when the appendix becomes inflamed. The appendix is a small, finger-shaped pouch located in the lower right abdomen. While its exact function is still unknown, it is believed to play a role in the immune system. When the appendix becomes blocked, usually by fecal matter, it can lead to an infection and inflammation.
Symptoms of Appendicitis
Appendicitis typically presents with the following symptoms:
- Pain in the lower right abdomen: The pain usually starts around the belly button and then moves to the lower right abdomen. It may worsen with movement, coughing, or sneezing.
- Nausea and vomiting: Many individuals with appendicitis experience nausea, which may be accompanied by vomiting.
- Loss of appetite: Appendicitis can cause a decreased appetite or complete loss of appetite.
- Fever and chills: In some cases, appendicitis can lead to a low-grade fever and chills.
- Changes in bowel habits: You may experience changes in your bowel movements, such as diarrhea or constipation.
It’s important to note that symptoms can vary from person to person, and some individuals may not exhibit all of these symptoms. If you suspect you have appendicitis, it is crucial to seek medical attention promptly.
Surgical Interventions for Appendicitis
The primary treatment for appendicitis is surgical removal of the inflamed appendix, known as an appendectomy. At Lenox Hill Surgeons, our experienced general surgeons offer two main approaches to appendix surgery:
Open Appendectomy
During an open appendectomy, the surgeon makes an incision in the lower right abdomen and removes the inflamed appendix. This traditional approach allows direct visualization of the appendix and surrounding tissues. While it requires a larger incision, open appendectomy remains a reliable and effective surgical intervention.
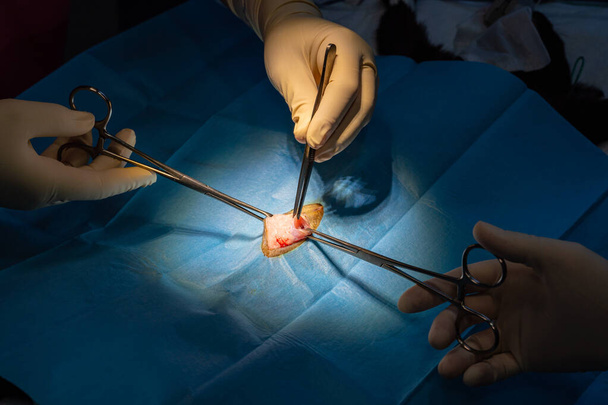
Laparoscopic Appendectomy
Laparoscopic appendectomy is a minimally invasive technique that utilizes several small incisions and a laparoscope, a thin tube with a camera, to guide the surgical procedure. The surgeon inserts specialized instruments through the small incisions to remove the appendix. Laparoscopic appendectomy offers several advantages, including smaller incisions, less post-operative pain, faster recovery, and reduced scarring.
The choice between an open or laparoscopic appendectomy depends on factors such as the severity of the appendicitis, the patient’s overall health, and the surgeon’s recommendation. At Lenox Hill Surgeons, our skilled surgeons will assess your individual case and determine the most suitable approach for your appendix surgery.
Appendicitis and Surgical Intervention Services at Lenox Hill Surgeons
When it comes to appendix surgery, trust the expertise of the surgeons at Lenox Hill Surgeons. Our dedicated team is committed to providing exceptional surgical care with a patient-centric approach. We prioritize your well-being and strive for optimal surgical outcomes.
Contact us today to schedule a consultation and experience the expertise of our renowned surgeons:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Colon Surgery: Exploring Procedures for Colon Conditions
In this article, we will explore different procedures for colon conditions and their importance in restoring health and well-being. The colon, also known as the large intestine, plays a vital role in the digestive process. However, various conditions can affect the colon, such as colon cancer, diverticulitis, and inflammatory bowel disease. When conservative treatments fail to provide relief or manage these conditions effectively, colon surgery may be necessary. At Lenox Hill Surgeons, a leading general surgery practice in New York City, our team of expert surgeons specializes in a range of colon surgeries.
Procedures for Colon Conditions
1. Colectomy: Removing Diseased Portions of the Colon
Colectomy is a common surgical procedure that involves the removal of diseased portions of the colon. It is often performed to treat conditions such as colon cancer, ulcerative colitis, or Crohn’s disease. During a colectomy, the surgeon carefully removes the affected segment of the colon and reconnects the remaining healthy portions. In some cases, a temporary or permanent colostomy may be necessary to redirect waste through an opening in the abdominal wall.
2. Colostomy: Creating an Opening in the Abdominal Wall
Colostomy is a surgical procedure in which an opening is created in the abdominal wall, allowing waste to bypass the lower part of the colon and exit the body. It is typically performed when the lower part of the colon or rectum is removed or bypassed, as in cases of rectal cancer or severe inflammatory bowel disease. A colostomy may be temporary or permanent, depending on the specific condition and treatment plan. It requires the use of a colostomy bag to collect waste, which can be emptied or replaced as needed.
3. Robotic-Assisted Colon Surgery: Precision and Enhanced Recovery
Robotic-assisted colon surgery is an advanced minimally invasive technique that utilizes robotic technology to assist the surgeon during the procedure. It offers several advantages, including enhanced precision, improved visualization, and smaller incisions. The robotic system allows for greater dexterity and maneuverability, facilitating intricate surgical tasks with greater accuracy. Patients who undergo robotic-assisted colon surgery often experience faster recovery, reduced pain, and a shorter hospital stay compared to traditional open surgery.
4. Laparoscopic Colon Surgery: Minimally Invasive Approach
Laparoscopic colon surgery, also known as keyhole surgery, is a minimally invasive procedure that utilizes small incisions and specialized surgical instruments. The surgeon inserts a laparoscope, a thin tube with a camera, through one of the incisions to visualize the surgical area. Additional instruments are inserted through the other small incisions to perform the surgery. Laparoscopic colon surgery offers several benefits, including reduced post-operative pain, shorter recovery time, and minimal scarring.
Expert General Surgical Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we understand the importance of personalized care and expertise when it comes to colon surgery. Our team of experienced general surgeons is committed to providing exceptional surgical services, utilizing advanced techniques and innovative technology. We prioritize patient well-being, ensuring comprehensive evaluations, tailored treatment plans, and compassionate care throughout the surgical journey.
Contact us today to schedule a consultation with our renowned surgeons:
Contact Information:
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Choosing the Right General Surgeon: Key Questions to Ask
If you need to get surgery, when it comes to your health and well-being, choosing the right general surgeon is crucial. Whether you require a routine procedure or a complex surgery, finding a skilled and experienced surgeon is essential for optimal outcomes. At Lenox Hill Surgeons, a leading general surgery practice in New York City, we understand the importance of selecting the right surgeon. In this article, we’ll provide you with key questions to ask when choosing a general surgeon to ensure you make an informed decision.

1. Are you board-certified in general surgery?
Board certification demonstrates that the surgeon has undergone rigorous training and has met the highest standards of knowledge and skill in the field of general surgery. It’s essential to ensure that the surgeon you choose is certified by the appropriate board, such as the American Board of Surgery.
2. What is your experience and specialization?
Inquire about the surgeon’s experience and expertise in performing the specific procedure you require. Ask how frequently they perform the procedure and if they have any sub-specializations within general surgery. A surgeon with significant experience and specialization in the procedure you need will likely yield better outcomes.
3. Where will the surgery be performed?
Ask about the surgical facility where the procedure will take place. Ensure that the facility is accredited and equipped with state-of-the-art technology. Lenox Hill Surgeons operates in a modern facility with advanced surgical equipment and a highly trained staff, ensuring the highest quality of care.
4. What is the success rate for this procedure?
Inquire about the surgeon’s success rate for the specific procedure you require. A skilled surgeon will have a track record of successful outcomes. While no surgery is without risks, understanding the surgeon’s success rate can help you assess their competence and expertise.
5. What are the potential risks and complications?
A competent surgeon will be transparent about the potential risks and complications associated with the procedure. Ask about the specific risks and what measures will be taken to minimize them. Understanding the potential complications allows you to make an informed decision and be prepared for the recovery process.
 6. What is the recovery process like?
6. What is the recovery process like?
Understanding the recovery process is crucial for planning and managing your expectations. Ask about the expected recovery time, any post-operative care requirements, and restrictions on activities during the healing period. A good surgeon will provide clear instructions and support throughout the recovery process.
7. Can I see testimonials or speak to previous patients?
Requesting testimonials or the opportunity to speak to previous patients can provide valuable insights into the surgeon’s skill, bedside manner, and patient satisfaction. Hearing from others who have undergone similar procedures can help you feel more confident in your choice.
8. Do you accept my insurance?
Ensure that the surgeon and the practice accept your insurance coverage. Contact your insurance provider to verify the surgeon’s participation in your plan and to understand any potential out-of-pocket expenses.
Choosing the Right General Surgeon: Expert General Surgical Services at Lenox Hill Surgeons
At Lenox Hill Surgeons, we understand the importance of choosing the right general surgeon for your healthcare needs. Our team of skilled and experienced surgeons is committed to providing exceptional surgical care with a patient-centric approach. Contact us today to schedule a consultation and experience the expertise of our renowned surgeons.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Hernia Repair: Types, Symptoms, and Treatment Options
If you’re experiencing discomfort or a noticeable bulge in your abdomen, it could be a hernia. Hernias occur when an organ or tissue protrudes through a weak spot in the surrounding muscle or connective tissue. They can cause pain, discomfort, and affect your quality of life. At Lenox Hill Surgeons, a leading general surgery practice in New York City, our skilled surgeons specialize in hernia repair. In this guide, we’ll explore different types of hernias, their symptoms, and the available hernia repair options.
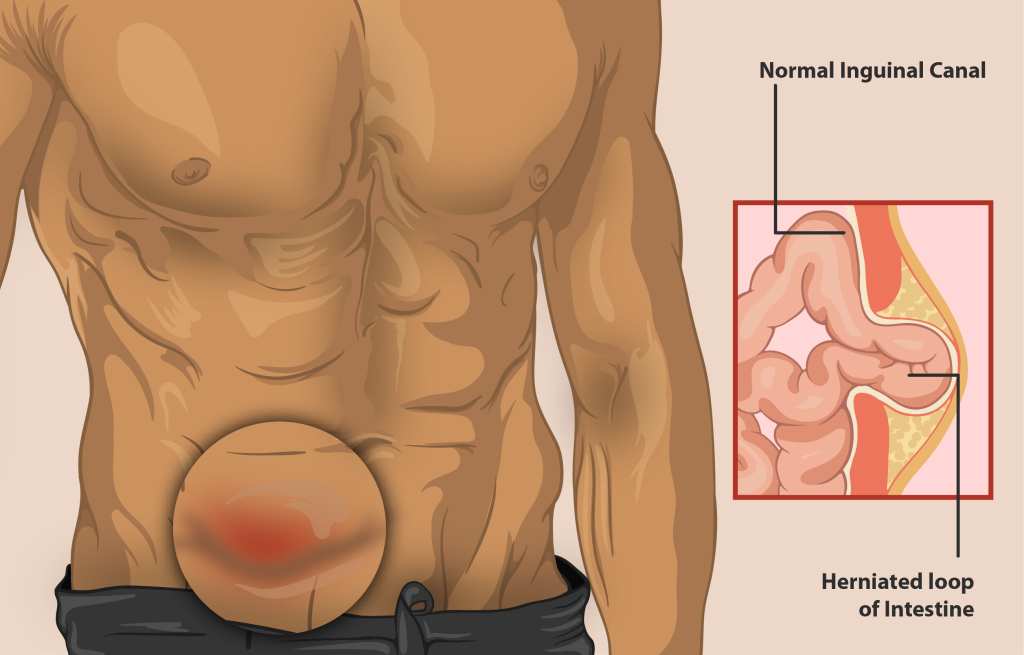
Types of Hernias
There are several types of hernias that can occur in different areas of the body. The most common types include:
- Inguinal Hernia: This occurs when a portion of the intestine or abdominal tissue protrudes through the inguinal canal in the groin area. It is more common in men than women.
- Femoral Hernia: Similar to an inguinal hernia, a femoral hernia also occurs in the groin area but is more common in women. It happens when a loop of intestine protrudes through the femoral canal.
- Incisional Hernia: This type of hernia develops at the site of a previous surgical incision. It can occur due to weak scar tissue, especially if the incision was large or did not heal properly.
- Umbilical Hernia: Umbilical hernias are common in infants but can also affect adults. They happen when the intestine or fatty tissue protrudes through a weakness near the navel.
- Hiatal Hernia: Unlike the previous types, hiatal hernias occur in the upper part of the stomach. They develop when a portion of the stomach protrudes through the diaphragm into the chest cavity.
Symptoms of Hernias
Hernias can present various symptoms, including:
- A visible or palpable bulge or lump in the affected area
- Pain or discomfort, especially when lifting heavy objects or straining
- Burning or aching sensation at the site of the hernia
- Nausea, vomiting, or difficulty with bowel movements in some cases
- Discomfort or pain during physical activity or prolonged standing
It’s important to note that not all hernias cause symptoms. Some hernias may be asymptomatic but still require medical attention to prevent potential complications.
Hernia Repair: Treatment Options
The primary treatment for hernias is surgical repair. At Lenox Hill Surgeons, our experienced general surgeons offer several approaches to hernia repair, including:
- Open Hernia Repair: This traditional approach involves making an incision near the hernia site to access and repair the weakened area. The surgeon may use sutures or a mesh patch to reinforce the muscle or tissue.
- Laparoscopic Hernia Repair: A minimally invasive technique, laparoscopic hernia repair utilizes small incisions and a laparoscope, a thin tube with a camera, to guide the repair process. The surgeon inserts instruments through these small incisions and repairs the hernia using sutures or a mesh patch.
- Robotic-Assisted Hernia Repair: Robotic surgery combines the precision of robotics with the skills of the surgeon. This approach allows for enhanced dexterity and visualization during the repair process, resulting in excellent outcomes.
The choice of the surgical technique depends on several factors, including the type and size of the hernia, the patient’s overall health, and the surgeon’s expertise. During a consultation at Lenox Hill Surgeons, our surgeons will discuss the most suitable approach for your specific case.
Expert Hernia Repair Surgery at Lenox Hill Surgeons
If you’re experiencing symptoms of a hernia or have been diagnosed with one, seek prompt medical attention. At Lenox Hill Surgeons, our team of skilled general surgeons is committed to providing exceptional hernia repair services. We prioritize patient safety, comfort, and long-term success.
Contact us today to schedule a consultation and discuss your hernia repair options.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Guide to General Surgery in Manhattan: What You Need to Know
Guide to General Surgeries in NYC: Restoring Health through Surgical Interventions
If you’re considering general surgery in Manhattan, it’s essential to be well-informed about the various procedures available, their benefits, and what to expect throughout the process. At Lenox Hill Surgeons, a leading general surgery practice in New York City, we understand the importance of providing comprehensive information to help you make informed decisions about your healthcare. In this guide, we’ll walk you through the essential aspects of general surgeries, helping you understand the common procedures, their significance in addressing specific conditions, and what you can expect during the surgical process.

Hernia Repair: Types, Symptoms, and Treatment Options
One common general surgery procedure is hernia repair. Hernias occur when an organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue. They can cause discomfort, pain, and potential complications if left untreated. Skilled surgeons employ various hernia repair techniques, such as laparoscopic or robotic-assisted approaches, tailored to your specific condition. Understanding the different types of hernias, their symptoms, and available treatment options can empower you to seek timely medical intervention.
Appendix Surgery: Understanding Appendicitis and Surgical Interventions
Appendicitis is another prevalent condition that often requires surgery. It occurs when the appendix becomes inflamed, leading to severe abdominal pain and other symptoms. If left untreated, it can result in a ruptured appendix, which is a medical emergency. Prompt surgical intervention is crucial to alleviate your pain and prevent further complications. Learning about the causes, symptoms, and surgical approaches for appendicitis can help you recognize the signs and seek appropriate medical care.
Colon Surgery: Exploring Procedures for Colon Conditions
Colon surgery is performed to address various conditions affecting the large intestine, including colon cancer, diverticulitis, and inflammatory bowel disease. Skilled surgeons utilize advanced techniques, such as minimally invasive laparoscopic surgery, to remove diseased portions of the colon and restore normal bowel function. Understanding the different colon conditions, their implications, and the available surgical procedures can help you navigate your treatment journey with confidence.
Gallbladder Surgery: Common Disorders and Surgical Solutions
Gallbladder surgery, often known as cholecystectomy, is performed to treat gallbladder-related disorders, such as gallstones or inflammation. Skilled surgeons are well-versed in laparoscopic gallbladder removal, a minimally invasive approach that offers smaller incisions, reduced scarring, and faster recovery compared to traditional open surgery. Understanding the common gallbladder disorders, their symptoms, and the surgical solutions available can empower you to make informed decisions about your health.
Adrenal Gland Disorders: Surgical Approaches and Treatment Considerations
When adrenal gland disorders, such as tumors or hormone imbalances, require surgical intervention, experienced surgeons employ advanced techniques to ensure precise removal of tumors and effective management of hormone-related conditions. Understanding adrenal gland disorders, their impact on overall health, and the surgical approaches available can help you navigate treatment options and make informed decisions about your care.
Liver Surgery: Procedures for Liver Diseases and Tumors
Liver surgery encompasses a wide range of procedures, including liver resection, transplantation, and treatment of liver tumors. Collaborating closely with liver specialists and oncologists, experienced surgeons develop comprehensive treatment strategies tailored to your specific needs. Understanding the different liver diseases, tumors, and the surgical interventions available can provide you with the knowledge necessary to make informed decisions about your liver health.
Esophagus Surgery: Addressing Esophageal Conditions and Surgical Treatments
Esophagus surgery is performed to treat conditions affecting the esophagus, such as gastroesophageal reflux disease (GERD), esophageal cancer, and swallowing disorders. Skilled surgeons specialize in various esophagus surgeries, including fundoplication for GERD and minimally invasive procedures for cancer. Understanding esophageal conditions, their impact on daily life, and the surgical treatments available can help you navigate your treatment journey and find relief.
Stomach Surgery: Surgical Procedures for Gastric Disorders
Stomach surgery encompasses a range of procedures, including gastric bypass for weight loss and treatment of gastric ulcers or tumors. Skilled surgeons are proficient in performing stomach surgeries utilizing the latest techniques. Understanding the different gastric disorders, their impact on overall health, and the surgical procedures available can help you make informed decisions about your treatment and well-being.
Pancreas Surgery: Management of Pancreatic Diseases through Surgery
When pancreatic diseases, such as pancreatic cancer or pancreatitis, necessitate surgical intervention, experienced surgeons employ cutting-edge techniques to optimize outcomes. Equipped with state-of-the-art facilities and a multidisciplinary approach, skilled surgeons provide exceptional care for patients requiring pancreas surgery. Understanding pancreatic diseases, their implications, and the surgical interventions available can empower you to take an active role in your treatment.
Small Intestine Surgery: Treatment Options for Intestinal Disorders
Small intestine surgery addresses a variety of conditions, such as Crohn’s disease, bowel obstructions, and small intestine tumors. Skilled general surgeons specialize in small intestine surgeries, employing advanced techniques to restore intestinal function and alleviate symptoms. Understanding the different intestinal disorders, their impact on daily life, and the available treatment options can help you navigate your treatment journey with confidence.
Spleen Surgery: Surgical Interventions for Splenic Conditions
Spleen surgery may be necessary for the treatment of various splenic conditions, such as ruptured spleen or enlarged spleen due to disease. Experienced surgeons possess extensive expertise in performing spleen surgeries, utilizing both traditional and minimally invasive approaches. Understanding splenic conditions, their implications, and the surgical interventions available can help you make informed decisions about your treatment and well-being.
Soft Tissue & Skin Surgery: Procedures for Lesions, Tumors, and Infections
In addition to internal surgeries, skilled surgeons also specialize in soft tissue and skin surgeries. They offer expert surgical interventions for skin lesions, tumors, and infections, ensuring optimal cosmetic and functional results. Trust experienced surgeons to provide personalized care and effective treatment for your soft tissue and skin conditions.
At Lenox Hill Surgeons, we are dedicated to delivering the highest standard of care, utilizing advanced surgical techniques, and prioritizing patient well-being. If you’re seeking expert general surgical services in Manhattan, contact us today.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-846-1136
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Types of Hernias: Ventral Hernia
What is a ventral hernia? Hernias can occur in any part of your body. Each different type of hernia gets its name depending on where it occurs. In its true nature, a hernia refers to a condition in which the internal muscle tissue weakens or becomes thin. In this case, the abdominal or whichever muscle… Continue Reading
Types of Hernias: Inguinal Hernia
An Inguinal Hernia is a condition in which one spot of the abdominal muscle weakens, and this causes muscle tissue to protrude outwards, causing a bulge. Therefore, you can call this hernia a protrusion bulge as well. It is the projection of an organ through the muscle tissues that make up the body wall. Mostly,… Continue Reading
General Surgery: Colon Cancer
People with colon cancer mostly have to undergo general surgery. It is the primary treatment for people with early stages of colon cancer. Furthermore, there are different types of colon surgeries. The doctors choose to perform between each of the surgery by considering certain factors. These factors involve the severity of cancer, location of the… Continue Reading
Do you Think you May Have a Hernia?
Do you think you may have a hernia? Read on to learn all about what hernias are and how they are caused. Many people classify Hernias into different kinds, Inguinal, Femoral, Incisional, and Umbilical. However, few understand the exact occurrence of the Hernia. You will find most of the hernia occurrences in the abdominal regions… Continue Reading
Inguinal Hernia
An Inguinal Hernia is a condition in which one spot of the abdominal muscle weakens, and this causes muscle tissue to protrude outwards, causing a bulge. Therefore, you can call this hernia a protrusion bulge as well. It is the projection of an organ through the muscle tissues that make up the body wall. Mostly,… Continue Reading
Pancreas Disease and Surgery
This article will cover important information about pancreas disease and surgery. The pancreas is a pivotal organ of the human body. It is responsible for the regulation of vital enzymes inside the body. These enzymes help regulate important chemical processes inside the body. Furthermore, it also produces insulin, which is an essential chemical that controls… Continue Reading
Hiatal Hernia
What is a hiatal hernia? Hernias are disruptive conditions in which the tissue linings or muscle walls become unable to hold the tissue cavities in place. It happens due to the weakening or thinning down of muscle tissue. Abdominal hernias are the most common type of hernias. Hernias come in two forms, either external or… Continue Reading
All About Appendix Surgery
Appendix surgery, more commonly known as appendectomy, is the surgical removal of an appendix from inside a person’s body. This rather common procedure has no negative implications and is a result of very few complications. The appendix is a small pouch-shaped organ inside our body. It takes space in the lower right side of the… Continue Reading
The Colon: Common Problems & Surgery
What surgery and problems are common to the colon? The colon is a long tube-like organ that makes up most of the large intestine. It is one of the major parts of the digestive tract, responsible for the formation and disposal of our indigested stool. Once the food enters into the small intestine and all… Continue Reading
Gallbladder Disease: Will You Need Serious Surgery?
Do you need serious surgery for gallbladder disease? A gallbladder is an organ that aids a person’s digestion by storing bile and releasing it in the small intestine. It’s a small organ located right under the liver, with a highly purposeful functionality in the body. Bile is a yellowish liquid that the liver makes and… Continue Reading
Ventral Hernia Causes, Symptoms & Treatment
What is a ventral hernia? Hernias can occur in any part of your body. Each different type of hernia gets its name depending on where it occurs. In its true nature, a hernia refers to a condition in which the internal muscle tissue weakens or becomes thin. In this case, the abdominal or whichever muscle… Continue Reading
The Esophagus: Common Problems & Surgery
What are the common problems and surgery of the esophagus? Esophagus refers to the tube that takes food that you put in your mouth and sends it down the digestive tract for absorption. Through peristalsis, the esophagus ensures that the food bolus travels smoothly down to your stomach, where it becomes ready for digestion. However,… Continue Reading