CALL TODAY 646-846-1136 | EMAIL
Surgical Experts Dedicated to Improving Lives
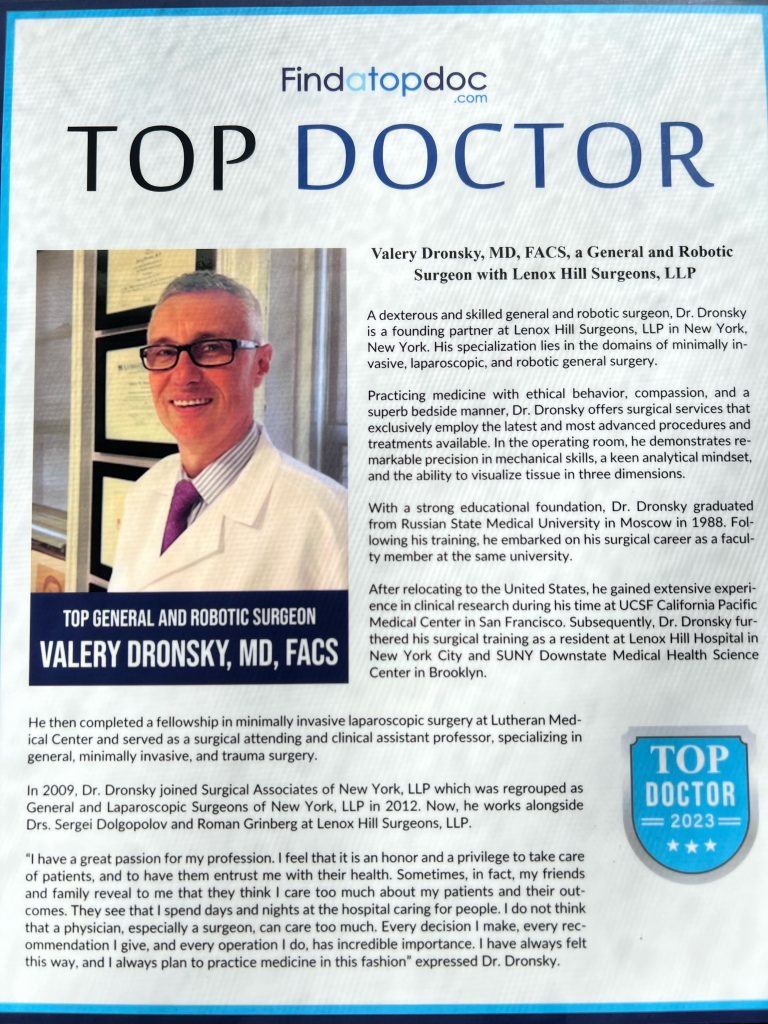
At Lenox Hill Minimally Invasive Surgery PLLC, Dr. Valery Dronsky and his staff of medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments. We specialize in general surgery, including extensive experience in performing hernia repair surgery. Our expertise is in minimally invasive surgery and robotic surgery. Minimally invasive and robotic surgery often allow patients to experience easier recovery than traditional open surgery. They also allow for more precise and less traumatic surgery. When robotic and minimally invasive surgery is not an option, we are also skilled and experienced in traditional open surgical procedures.
Dr. Dronsky is an experienced and highly skilled surgeon having undergone extensive training in school, residency and fellowships. He practices medicine with ethical behavior, compassion and superb bedside manner. In the operating room he exhibits precision mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These innate and learned skills allow Dr. Dronsky to be one of the most dexterous and skilled professionals in New York City and the Country.
Call us: 646-846-1136
PATIENT TESTIMONIALS
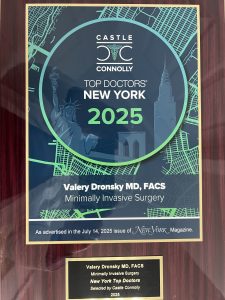
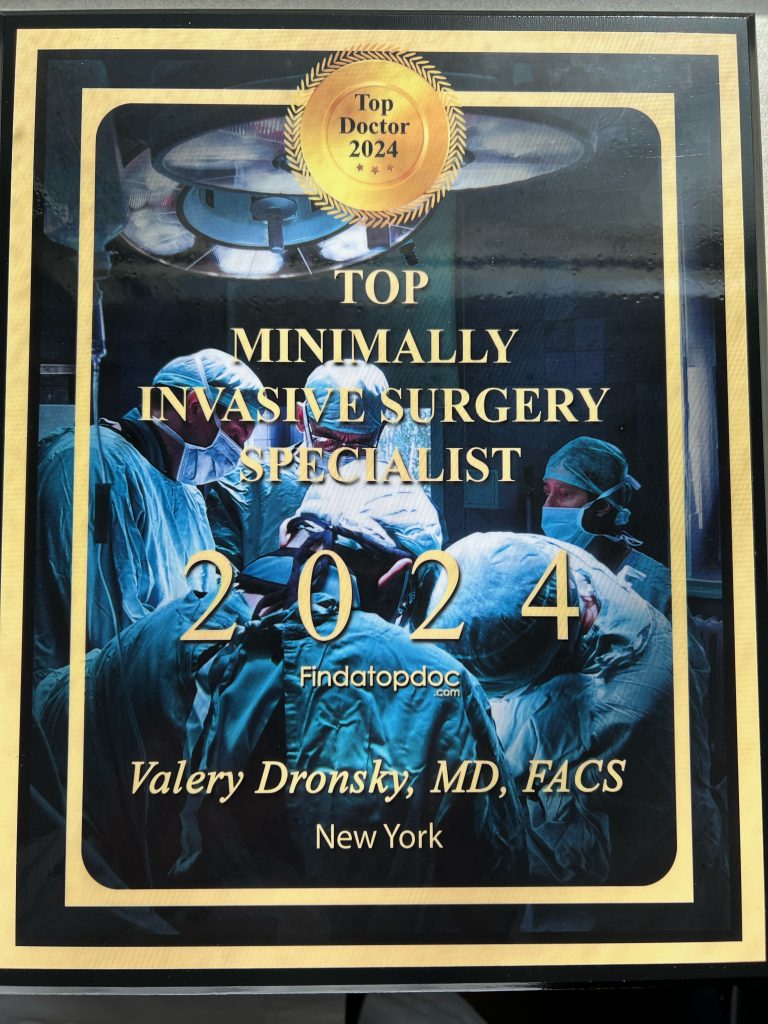
Recent Awards
We are honored and deeply appreciative to have consistently received prestigious awards and recognition year after year, establishing us as one of New York’s foremost hospitals for a wide range of general surgeries, safety measures, specialized procedures, and overall excellence in healthcare. At Lenox Hill Minimally Invasive Surgery, our unwavering commitment lies in delivering exceptional care and unwavering support to our patients, guaranteeing their safety and successful recovery throughout their entire surgical experience.
Hospital Quality Awards
 America’s 50 Best Hospitals Award™ (2023, 2022)
America’s 50 Best Hospitals Award™ (2023, 2022)
Top 1% in the nation for providing the highest clinical quality year over year.

America’s 100 Best Hospitals Award™ (2021)
Top 2% in the nation for consistently delivering clinical quality year over year.

America’s 250 Best Hospitals Award™ (2023, 2022, 2021)
Top 5% in the nation for consistently delivering clinical quality.

Patient Safety Excellence Award™ (2023, 2022)
Top in the nation for providing excellence in patient safety by preventing infections, medical errors, and other preventable complications.
Specialty Clinical Quality Awards

America’s 100 Best Hospitals for Cardiac Care Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in heart bypass surgery, coronary interventional procedures, heart attack treatment, heart failure treatment, and heart valve surgery.

America’s 100 Best Hospitals for Coronary Intervention Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in coronary intervention procedures (angioplasty with stent).

America’s 100 Best Hospitals for Prostate Surgery Award™ (2023, 2022, 2021)
Superior clinical outcomes in prostate removal surgery and transurethral resection of the prostate.
Click to see all of our Healthgrades best doctors awards


Visit our main website at www.LenoxHillMinimallyInvasiveSurgery.com
Blog Posts are Below:
Tag Archives: Laparoscopic surgery
Understanding Laparoscopic Surgery: Minimally Invasive Procedures in Manhattan
In this informative article, we will explore laparoscopic surgery, its advantages, and the range of procedures it encompasses. Advancements in surgical techniques have revolutionized the field of medicine, allowing for more precise and minimally invasive procedures. Laparoscopic surgery, also known as keyhole surgery, has gained popularity for its numerous benefits compared to traditional open surgery. Lenox Hill Minimally Invasive Surgery, a leading general surgery practice in Manhattan, specializes in this type of surgery, offering patients advanced and minimally invasive treatment options.

What is Laparoscopic Surgery?
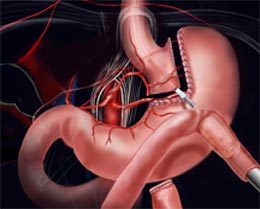
Laparoscopic surgery is a minimally invasive surgical technique that utilizes small incisions and specialized surgical instruments. It involves the use of a laparoscope, a thin tube with a camera and light source, which allows the surgeon to visualize the surgical area in high definition. The images captured by the laparoscope are projected onto a monitor, guiding the surgeon throughout the procedure.
The Advantages of Laparoscopic Surgery
Laparoscopic surgery offers several advantages over traditional open surgery:
1. Minimally Invasive:
The use of small incisions results in less tissue trauma, leading to reduced post-operative pain, less scarring, and faster recovery times compared to open surgery.
2. Reduced Blood Loss:
Laparoscopic procedures involve precise incisions and the use of specialized instruments, which help minimize blood loss during surgery.
3. Enhanced Visualization:
The laparoscope provides a magnified and detailed view of the surgical site, allowing surgeons to perform intricate procedures with improved precision.
4. Shorter Hospital Stay:
Laparoscopic surgery often allows for shorter hospital stays, enabling patients to return to their daily activities and routines more quickly.
5. Quicker Recovery:
With reduced post-operative pain and smaller incisions, patients experience faster recovery times, allowing them to resume their regular activities sooner.
Common Laparoscopic Procedures
Laparoscopic surgery is employed in various general surgical procedures. Here are some common examples:
1. Laparoscopic Cholecystectomy:
This procedure involves the removal of the gallbladder through small incisions. Laparoscopic cholecystectomy is a highly effective treatment for gallstones and gallbladder disease.
2. Laparoscopic Appendectomy:
Appendectomy is the surgical removal of the appendix. Laparoscopic appendectomy is the preferred approach for most cases of appendicitis, resulting in less pain, faster recovery, and minimal scarring.
3. Laparoscopic Hernia Repair:
Laparoscopic techniques are commonly used to repair different types of hernias, such as inguinal, femoral, or umbilical hernias. This approach provides excellent results with minimal post-operative discomfort.
4. Laparoscopic Colon Resection:
Laparoscopic colon resection involves the removal of a portion of the colon affected by conditions such as colon cancer, diverticulitis, or inflammatory bowel disease. It offers benefits such as reduced pain and faster recovery.
Expert Laparoscopic Surgery Services at Lenox Hill Minimally Invasive Surgery
At Lenox Hill Minimally Invasive Surgery, we understand the importance of advanced surgical techniques in improving patient outcomes and quality of life. Our skilled team of general surgeons specializes in laparoscopic surgery, utilizing the latest technologies and techniques to ensure the best results for our patients.
Contact us today to schedule a consultation and benefit from the expertise of our renowned surgeons:
Contact Information:
LENOX HILL MINIMALLY INVASIVE SURGERY
117 E 77th Street
Suite 1A
New York, NY 10075
646-846-1136
admin@lenoxmis.com
Visit our website for more information: https://lenoxhillminimallyinvasivesurgery.com/
Appendicitis
Appendicitis is one of the most common factors responsible for abdominal pain, which can lead to surgery. More than 5 percent of people in the US experience appendicitis at some point. However, the pain most often occurs in people aged between 10 and 30.
Appendicitis is the inflammation of a 3.5-inch long appendix tube that protrudes from the large intestine. The condition calls for an immediate treatment, most probably surgery to remove the appendix.
Leaving an inflamed appendix untreated will cause the tube to burst. Thus, the inflamed appendix may start spilling infectious bacteria into the abdominal cavity. And, it may prove fatal sometimes.
Symptoms of Appendicitis
Usually, the first sign of appendicitis is a sudden pain that begins in the upper abdomen and radiates to the lower right portion of the abdomen. The pain may become excruciating when you cough or walk.
The inflamed appendix may cause you to lose appetite, or you may feel nausea or vomiting as soon as the pain begins. Abdominal bloating and low-grade fever, usually 99 – 102 Fahrenheit, may also serve as signs of the inflammation of appendix.
The other symptoms of appendicitis include severe cramps, dull or sharp pain in the back, rectum, or the lower or upper abdomen.
What Causes Appendicitis?
While the root cause of appendicitis remains unknown in most of the cases, doctors believe that inflammation occurs when the appendix is blocked. The obstruction in the lining may occur due to hardened stool, intestinal worms, enlarged lymphoid follicles or cancer.
The blockage in the appendix results in an infection, which may multiply the bacteria. Thus, it leads to the swelling and formation of pus in the appendix, thereby causing inflammation. You may also feel severe pain in the abdominal region, and if not treated timely, the appendix may rupture.
Appendicitis’ Diagnosis
The symptoms of appendicitis are often confused with that of the gallbladder diseases, bladder or urine infection, intestinal infection, gastritis, and ovary problems. This makes the diagnosis of appendicitis tricky. Your doctor may conduct these tests for diagnosing the inflammation in the appendix.
- Examination of the abdominal region: This helps identify the stiffening of the abdominal muscles when the doctor applies pressure on the appendix.
- Rectal Exam: The doctor examines the lower rectum with a lubricated gloved finger.
- Blood Test: The blood tests show a high white blood cell count in the body, thereby indicating an infection.
- Urinalysis: The urine test helps rule out a urinary tract infection or a kidney stone as a possible cause of the pain.
- Imaging Tests: The doctor may require an abdominal X-ray, ultrasound, a CT scan, or an MRI of the patient for the diagnosis of appendicitis.
Treatment: Appendectomy
The standard treatment for all appendicitis is appendectomy, i.e., the removal of appendicitis. The doctor may either perform open surgery or a laparoscopic surgery depending on the severity of the problem.
During the open surgery, the doctor makes an incision, which is usually 2 to 4 inches long. Doctors perform this type of surgery when the appendix has ruptured, and an excess abscess or puss has formed around it. Thus, the doctor drains the fluid and cleans the abdominal cavity.
Once the infection is under control, the doctor may perform minimally invasive or laparoscopic surgery. The surgeon will use some incisions to insert surgical instruments and a video camera into the abdominal region to remove the appendix.
Final Word
Do not neglect the pain that you experience in your abdomen. It may be a sign of an inflamed appendix. If you do not go for a treatment promptly, it may cause your appendix to rupture. Contact Lenox Hill Minimally Invasive Surgery in NYC today and book an appointment with the experts of minimally invasive surgery.
Pancreas Surgery – NYC General Surgeon
Pancreas Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
 The pancreas being a key organ of the endocrine and digestive systems of the body is indispensable for the smooth functioning of the human body. Hence, a diseased condition of the pancreas, like a tumor, abscess or malignancy that causes pancreatitis and makes the dysfunctional organ calls for pancreatic surgery. There are different methods, or kinds of pancreas surgery and the type that a patient will have to opt for will depend upon whether his or her pancreatitis is chronic or acute.
The pancreas being a key organ of the endocrine and digestive systems of the body is indispensable for the smooth functioning of the human body. Hence, a diseased condition of the pancreas, like a tumor, abscess or malignancy that causes pancreatitis and makes the dysfunctional organ calls for pancreatic surgery. There are different methods, or kinds of pancreas surgery and the type that a patient will have to opt for will depend upon whether his or her pancreatitis is chronic or acute.
More often than not, the condition or syndrome can be treated and managed without going for invasive intervention or surgery. Nevertheless, if an infection or degeneration of the pancreatic tissues becomes longstanding and acute, surgery is the only treatment option.
Steps
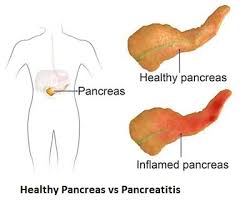 The most common pancreatic surgery procedures include minimally invasive pancreatic resection, spleen-preserving pancreatectomy, ‘The Whipple’, and Enucleation of pancreatic tumor.’ Minimally invasive pancreatic resection surgery is conducted laparoscopically giving the interventional radiologist or gastroenterologist good access to the abdomen via tiny keyhole notches. This surgical method is appropriate for patients having pancreatic cysts.
The most common pancreatic surgery procedures include minimally invasive pancreatic resection, spleen-preserving pancreatectomy, ‘The Whipple’, and Enucleation of pancreatic tumor.’ Minimally invasive pancreatic resection surgery is conducted laparoscopically giving the interventional radiologist or gastroenterologist good access to the abdomen via tiny keyhole notches. This surgical method is appropriate for patients having pancreatic cysts.
Spleen-preserving pancreatectomy is conducted laparoscopically where the pancreas is excised, but the spleen is kept intact for preserving its immunological functionality as well as minimize the risks of complications and infections in the future. The traditional pancreatectomy method entails the removal of the spleen along with the metastatic pancreas for reversing the spread of cancer. Nevertheless, if the surgery is carried out for a benign condition like pancreatic tumor or cyst, then spleen resection is not necessary.
Enucleation process is appropriate for dealing with benign or non-cancerous tumors where these are scraped out carefully instead of expurgating a large pancreatic section.
‘The Whipple’ surgery or ‘pancreaticoduodenectomy’ is the go-to procedure for treating pancreatic cancer and also for dealing with complications or abscesses related to the bile duct, intestine, and pancreas. The surgery where the top of the pancreas, bile duct, gallbladder, and duodenum are removed can be extremely complex and demanding, fraught with risks.
Benefits
If the surgery is for treating pancreatitis or tumors, then opting for laparoscopic surgery is the best option. In such a case, recuperation is faster necessitating a shorter hospital stay. However, if the surgery is for pancreatic cancer, then the operation lasts for several hours and the patient may have to be in the hospice for at least a week.
Complete recovery might take many weeks and even months. Benefits of going for a major pancreatic surgery are:-
- Best treatment technique for remedying cancer and reversing chronic pancreatitis
- Increased lifespan
- Digestive issues and complications associated with pancreas might be resolved post surgery
- Chemotherapy and radiotherapy for continued treatment in case cancer recurs
Side Effects
Pancreatic surgeries for dealing with cancer tend to be extremely complicated, and it is no wonder that such operations have a very high mortality rate. Nearly 50% of the patients report grave complications and about 2%-4% expire. The most common risks include:-
- Wound infection or cardiac infection
- Hemorrhage (bleeding)
- Leakage from pancreas from the point where it is linked with the intestine
- Allergic reaction to general anesthesia (very rare)
Precautions
Fully recuperating from a complex pancreas surgery takes time and the convalescing process could be exhausting, especially for older patients. You’ll be required to report to your surgeon 1-2 times in a month following your recovery. The doctor will evaluate your progress and may recommend CT or MRI scans, and blood tests to ensure that there is no recurrence of cancerous tumors or lesions.
Dietary and lifestyle changes to have to be made to maintain overall health and also to reduce the risks of relapse.
Prognosis
Pancreatic cancer and all other serious complications of the pancreas are, by and large, regarded as untreatable and hence incurable. Nevertheless, the mortality rates related to pancreatic cancer (post surgery) have steadily declined over the decades.
Concluding Remarks
Living without a pancreas can be a challenge for any individual. If you’re diagnosed with a tumor or inflammation of your pancreas, you can continue to live an almost normal life, provided you opt for an appropriate treatment plan and abide by our physician’s guidelines. If you’ve cancer, then surgical removal of the pancreas is the only option. However, you’ll have to keep your fingers crossed on whether cancer will recur or not.
References
- https://www.mayoclinic.org/tests-procedures/whipple-procedure/about/pac-20385054
- https://stanfordhealthcare.org/medical-treatments/c/cancer-surgery/types/complex-pancreatic-surgery.html
- https://www.mskcc.org/blog/drug-reduces-risk-serious-pancreatic-surgery-complication
- https://stanfordhealthcare.org/medical-treatments/p/pancreatic-surgery/types/spleen-preserving-pancreatectomy.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2023932/
- https://www.ariahealth.org/programs-and-services/surgery/general-surgery/pancreatic-surgery
- http://columbiasurgery.org/pancreas/what-expect-after-operation
- https://www.cancer.org/cancer/pancreatic-cancer/treating/surgery.html
- http://pancreatic.org/pancreatic-cancer/about-the-pancreas/prognosis/
Stomach Surgery: Gastric Bypass by NYC Top Surgeon
Stomach Surgery (Gastric Bypass): Steps, Benefits, Side-Effects, Precautions & Prognosis
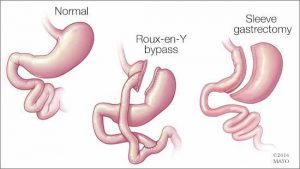 Gastric bypass is a type of surgical process chiefly carried out for treating a series of lifestyle conditions like type 2 diabetes, hypertension, obesity, and sleep apnea. These conditions more often than not occur concomitantly. The surgery is performed using a laparoscope (an elongated & slim tube featuring a high-resolution camera with intense light at the top) that is popped inside a slit made in the belly.
Gastric bypass is a type of surgical process chiefly carried out for treating a series of lifestyle conditions like type 2 diabetes, hypertension, obesity, and sleep apnea. These conditions more often than not occur concomitantly. The surgery is performed using a laparoscope (an elongated & slim tube featuring a high-resolution camera with intense light at the top) that is popped inside a slit made in the belly.
The laparoscope allows the surgeon to view the entire abdomen to restructure the small intestine to enable food to bypass the duodenum. This rearrangement leads to the body absorbing and assimilating fewer nutrients and calories, thereby enabling you to shed excess flab as well as stay fit and trim in the long run.
Steps
Stomach surgery is conducted in two distinct manners namely, open surgery and laparoscopy or laparoscopic surgery. In open surgery, the surgeon uses a scalpel for cutting open the stomach while in laparoscopy numerous small cuts are made in the abdomen. The end objective of both the types of surgery is to clearly view the digestive organs and the gastrointestinal tract and carry out the operation effectively.
The bypass surgery involves two necessary steps:
 1. The surgeon makes use of staples for sectioning the stomach into two halves: a larger bottom-half and a smaller upper half. The goal is to decrease the stomach’s size-the eventually reduced the volume of the upper section (known as pouch where the swallowed food will settle) will make you consume less, thereby letting you slim down.
1. The surgeon makes use of staples for sectioning the stomach into two halves: a larger bottom-half and a smaller upper half. The goal is to decrease the stomach’s size-the eventually reduced the volume of the upper section (known as pouch where the swallowed food will settle) will make you consume less, thereby letting you slim down.
2. The bypass surgery is performed in the 2nd step. The surgeon creates a notch in the pouch and links the jejunum (the initial part of the small intestine) with the opening. So, whatever you take will pass directly from the stomach’s upper pocket to the small intestine via this aperture, ultimately making you take in lesser calories.
On the whole, laparoscopy is preferred over general surgery as the former is less painful, involves shorter hospitalization and faster recuperation, and risks of infections are also lower.
Benefits
- The Roux-en-Y gastric bypass (the medical term for gastric surgery) results in considerable weight loss provided you fully abide by the instructions
- A good proportion of patients can maintain the postoperative bodyweight even 15-16 years after the surgery
- Optimal use of stored or available energy
- Feeling of fullness after taking a small meal and diminished appetite
Side effects
Like any other surgical procedure, gastric bypass is not without its complications and side effects. The following complications have been observed:
- Gastrointestinal/intra-abdominal hemorrhage
- Venous thromboembolism
- Increased risk of intra-abdominal infections like blisters and peritonitis
- Bowel obstruction
- A hernia
- Dumping of contents into the jejunum more frequently, especially when excessive foods or sugary foods are eaten
- Nutritional deficiencies (deficiency of calcium, iron, zinc, and folate as well as vitamins A, B1, and B12)
Precautions
There are certain precautions you’ll need to take once you’re released from the hospital following your surgery:
- Taking the prescribed medications on a regular basis
- Taking multivitamins, vitamin D, calcium, and vitamin B12 every day
- Taking balanced diets with limited consumption of calories
- Exercising daily for at least half an hour
- Remaining socially active
- Regular follow-up with the surgeon
Prognosis
Majority of individuals who opt for gastric surgery can lose 65% of their excess bodyweight. About 85% of those who undergo gastric bypass are successful in maintaining 50% of the excess weight they lost initially.
Concluding Remarks
Though gastric surgery is a practical solution for getting rid of inordinate bodyweight, the procedure can never be a panacea for obesity. If you wish to keep your weight under check post surgery and lead a fulfilling, healthy life, you’ll need to make lifestyle changes as well as heed dietary and exercise guidelines. To know more about stomach surgery as well as to fix an appointment with our bariatric surgeon, you can send us an email or contact us via phone.
References
- https://bariatric.surgery.ucsf.edu/conditions–procedures/laparoscopic-gastric-bypass.aspx
- https://medlineplus.gov/ency/article/007199.htm
- https://asmbs.org/patients/bariatric-surgery-procedures
- https://www.healthline.com/health/laparoscopy
- https://obesitynewstoday.com/gastric-bypass-success-rate/
- https://www.ucsfhealth.org/education/life_after_bariatric_surgery/
- https://www.acefitness.org/education-and-resources/lifestyle/blog/896/after-gastric-bypass-surgery-are-there-specific-exercise-precautions-i-should-take
General Surgery
Here are some brief descriptions about the different types of general surgery we perform:
Laparoscopic surgery
This is a relatively new specialty dealing with minimal access techniques using cameras and small instruments inserted through 0.3 to 1 cm incisions. Robotic surgery is now evolving from this concept (see below). Gallbladders, appendices, and colons can all be removed with this technique. Hernias are now repaired mostly laparoscopically. Most bariatric surgery is performed laparoscopically.[citation needed] General surgeons that are trained today are expected to be proficient in laparoscopic procedures.
Colorectal surgery
General surgeons treat a wide variety of major and minor colon and rectal diseases including inflammatory bowel diseases (such as ulcerative colitis or Crohn’s disease), diverticulitis, colon and rectal cancer, gastrointestinal bleeding and hemorrhoids.
Endocrine surgery
General surgeons are trained to remove all or part of the thyroid and parathyroid glands in the neck and the adrenal glands just above each kidney in the abdomen. In many communities, they are the only surgeon trained to do this. In communities that have a number of subspecialists, other subspecialty surgeons may assume responsibility for these procedures.
Surgical oncology
Surgical oncologist refers to a general surgical oncologist (a specialty of a general surgeon), but thoracic surgical oncologists, gynecologist and so forth can all be considered surgeons who specialize in treating cancer patients. The importance of training surgeons who sub-specialize in cancer surgery lies in evidence, supported by a number of clinical trials, that outcomes in surgical cancer care are positively associated to surgeon volume—i.e., the more cancer cases a surgeon treats, the more proficient he or she becomes, and his or her patients experience improved survival rates as a result. This is another controversial point, but it is generally accepted—even as common sense—that a surgeon who performs a given operation more often, will achieve superior results when compared with a surgeon who rarely performs the same procedure. This is particularly true of complex cancer resections such as pancreaticoduodenectomy for pancreatic cancer, and gastrectomy with extended (D2) lymphadenectomy for gastric cancer. Surgical oncology is generally a 2 year fellowship following completion of a general surgery residency (5-7 years).