CALL TODAY 646-846-1136 | EMAIL
Surgical Experts Dedicated to Improving Lives
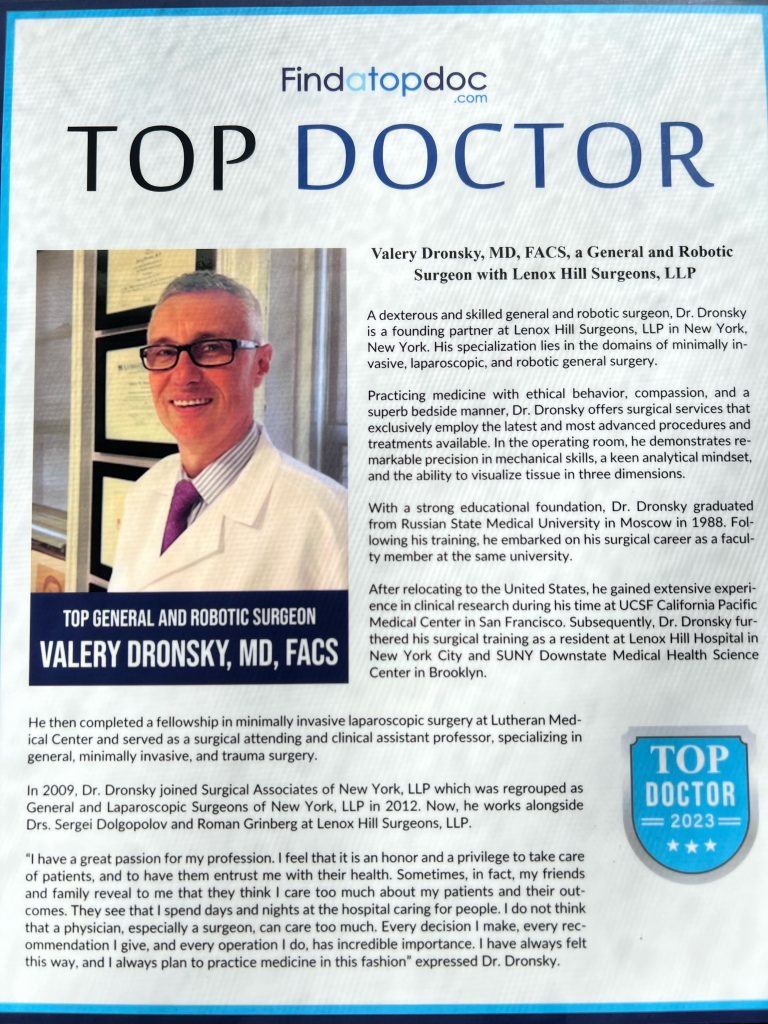
At Lenox Hill Minimally Invasive Surgery PLLC, Dr. Valery Dronsky and his staff of medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments. We specialize in general surgery, including extensive experience in performing hernia repair surgery. Our expertise is in minimally invasive surgery and robotic surgery. Minimally invasive and robotic surgery often allow patients to experience easier recovery than traditional open surgery. They also allow for more precise and less traumatic surgery. When robotic and minimally invasive surgery is not an option, we are also skilled and experienced in traditional open surgical procedures.
Dr. Dronsky is an experienced and highly skilled surgeon having undergone extensive training in school, residency and fellowships. He practices medicine with ethical behavior, compassion and superb bedside manner. In the operating room he exhibits precision mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These innate and learned skills allow Dr. Dronsky to be one of the most dexterous and skilled professionals in New York City and the Country.
Call us: 646-846-1136
PATIENT TESTIMONIALS
Recent Awards
We are honored and deeply appreciative to have consistently received prestigious awards and recognition year after year, establishing us as one of New York’s foremost hospitals for a wide range of general surgeries, safety measures, specialized procedures, and overall excellence in healthcare. At Lenox Hill Minimally Invasive Surgery, our unwavering commitment lies in delivering exceptional care and unwavering support to our patients, guaranteeing their safety and successful recovery throughout their entire surgical experience.
Hospital Quality Awards
 America’s 50 Best Hospitals Award™ (2023, 2022)
America’s 50 Best Hospitals Award™ (2023, 2022)
Top 1% in the nation for providing the highest clinical quality year over year.

America’s 100 Best Hospitals Award™ (2021)
Top 2% in the nation for consistently delivering clinical quality year over year.

America’s 250 Best Hospitals Award™ (2023, 2022, 2021)
Top 5% in the nation for consistently delivering clinical quality.

Patient Safety Excellence Award™ (2023, 2022)
Top in the nation for providing excellence in patient safety by preventing infections, medical errors, and other preventable complications.
Specialty Clinical Quality Awards

America’s 100 Best Hospitals for Cardiac Care Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in heart bypass surgery, coronary interventional procedures, heart attack treatment, heart failure treatment, and heart valve surgery.

America’s 100 Best Hospitals for Coronary Intervention Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in coronary intervention procedures (angioplasty with stent).

America’s 100 Best Hospitals for Prostate Surgery Award™ (2023, 2022, 2021)
Superior clinical outcomes in prostate removal surgery and transurethral resection of the prostate.
Click to see all of our Healthgrades best doctors awards


Visit our main website at www.LenoxHillMinimallyInvasiveSurgery.com
Blog Posts are Below:
Tag Archives: Precautions
Dysphagia Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
Dysphagia Surgery
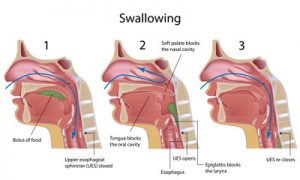 Some functional and anatomical abnormalities of the esophagus or the pharynx can cause dysphagia which is essentially a fancy medical term to indicate difficulty swallowing. This condition can be successfully treated by surgical procedures. Also, surgery is recommended when dysphagia is found to be associated with esophageal carcinoma, and compression of this organ due to other abnormalities or tumors in the chest. The surgical methods presently available are varied, and the choice of medical procedure is decided by the causative condition of dysphagia.
Some functional and anatomical abnormalities of the esophagus or the pharynx can cause dysphagia which is essentially a fancy medical term to indicate difficulty swallowing. This condition can be successfully treated by surgical procedures. Also, surgery is recommended when dysphagia is found to be associated with esophageal carcinoma, and compression of this organ due to other abnormalities or tumors in the chest. The surgical methods presently available are varied, and the choice of medical procedure is decided by the causative condition of dysphagia.
Steps
- The LES or lower esophageal sphincter is dilated in patients with achalasia. The doctor makes the patient swallow a tube having a balloon at its end. It is placed across the LES by means of an X-ray, and then the specialist blows the balloon all on a sudden. The objective is to stretch, rather tear, the sphincter. It can also be useful in treating Schatzki rings and strictures and other anatomical problems associated with
- In esophagomyotomy, the surgeon cuts the LES by making a large incision in the abdomen, or laparoscopically where small punctures are made in the chest or the abdomen of the patient.
Benefits
 For patients with severe dysphagia disorders, it may be necessary to bypass the pharynx entirely and the oral cavity to provide them with enteral nutrition. Surgical alternatives range from IOC or intermittent oroesophageal catheterization to PEG or percutaneous endoscopic gastronomy. Surgery for chronic cases of aspiration may include the following procedures:
For patients with severe dysphagia disorders, it may be necessary to bypass the pharynx entirely and the oral cavity to provide them with enteral nutrition. Surgical alternatives range from IOC or intermittent oroesophageal catheterization to PEG or percutaneous endoscopic gastronomy. Surgery for chronic cases of aspiration may include the following procedures:
- Medialization: It restores subglottic pressure and glottis closure during the swallow.
- Laryngeal suspension: The larynx is made to be rest in a comparatively protected place under the tongue.
- Laryngeal closure: The medical practitioner may perform it to shut the glottis off, and thus, provide ample protection for the airway while sacrificing the quality of phonation.
- Laryngotracheal separation-diversion: It may be opted to separate the alimentary tract from the airway.
Complications
The most commonly occurring complications are bleeding and perforation of cricopharyngeus. Dysphagia is typically reported after undergoing an ACS surgery, i.e., surgery of the anterior cervical spine. Although risk factors associated with dysphagia are published in the journals, they remain controversial to date.
Precautions
- The healthcare professional may prescribe making an alteration in food/liquid texture, temperature, or consistency.
- It is vital to ingest slowly and take smaller bites.
- The caregiver should also strictly adhere to the promoting strategies to ensure increased safety.
- It is crucial for one to maintain an appropriate positioning at the time of eating, and the ideal manner is to consume any liquid or food while holding an upright position, and also the chink being tucked a little at a right angle.
- An individual should continue to maintain the upright position even after finishing one’s meal, and should not make any attempt to alter the present position for a minimum of forty-five minutes post-consumption of the meals.
- If a person is found to be diagnosed with GERD also, then the head of the patient’s bed should be inclined at an angle of forty-five degrees.
- The care provider should always remember not to give an aspiration patient anything to consume a few hours before the bedtime.
- One should use medications that are meant to promote stomach emptying and reduce the reflux.
Prognosis
It is rather impossible for anyone to predict the outlook or prognosis for dysphagia in general, as numerous medical conditions can be held responsible for the symptoms associated with it. The outlook is case-dependent and is decided by the underlying medical issue/s of a patient.
Conclusion
Although dysphagia can appear to be frightening, this condition is not always necessarily chronic. The family physician should be consulted as soon as one starts experiencing any swallowing difficulties or other GERD (Gastroesophageal reflux disease) symptoms. The latter can be effectively treated with prescription drugs to reduce the amount of stomach acid.
Get in touch with us at 212-988-1136 or schedule an appointment to get immediate care and treatment for the condition.
References
Laparoscopic appendectomy – NYC General Surgeon
Laparoscopic appendectomy: Steps, Benefits, Side-Effects, Precautions & Prognosis
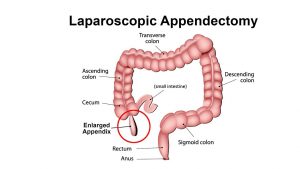
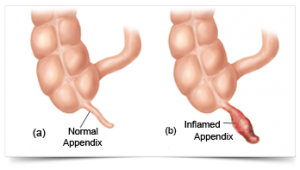
 The procedure of surgically removing the narrow, elongated tube attached to the colon-known as an appendix when it becomes diseased, inflamed or infected (appendicitis) is called appendectomy. It is normally carried out on an emergency basis as swollen appendicitis could burst if not excised, causing the clogged stool and bacteria to spread. It would eventually infect other gastrointestinal organs and lead to peritonitis-a life-threatening condition. A ruptured appendix could also create an abdominal abscess which is also a grave condition that could endanger your life.
The procedure of surgically removing the narrow, elongated tube attached to the colon-known as an appendix when it becomes diseased, inflamed or infected (appendicitis) is called appendectomy. It is normally carried out on an emergency basis as swollen appendicitis could burst if not excised, causing the clogged stool and bacteria to spread. It would eventually infect other gastrointestinal organs and lead to peritonitis-a life-threatening condition. A ruptured appendix could also create an abdominal abscess which is also a grave condition that could endanger your life.
Steps
Generally, two kinds of appendectomy are carried out to do away with appendicitis:
- The traditional ‘open appendectomy’
- Laparoscopic appendectomy (a more advanced form of surgery)
 Open appendectomy is more suitable for patients whose appendices have split open and also for those who have undergone abdominal surgery before.
Open appendectomy is more suitable for patients whose appendices have split open and also for those who have undergone abdominal surgery before.
A laparoscopic appendectomy, on the other hand, involves accessing the appendix via three tiny incisions or openings made in the lower abdomen. A cannula filled with carbon dioxide (a slender and small tube) is inserted through the openings for inflating the abdomen following which a laparoscope is slotted in.
A high-resolution camera fixed at the head of the laparoscope transmits the image to a display screen. The displayed images will clearly show the precise location of the appendix which in turn will help the surgeon to channelize the surgical instruments for ligation (of the appendix) and excising it. Keyhole surgery usually resorts if the patient happens to be overweight and aged.
Benefits
The specific benefits of laparoscopic appendectomy vary from one patient to another, depending upon his or her condition. Nevertheless, the common benefits entail:
- Short stay in the hospital
- Reduced postoperative pain
- Faster restoration of normal bowel function
- Speedier return to a normal lifestyle
Side Effects
The associated risk factors or complications are more or less the same for both laparoscopic appendectomy and open appendectomy. Following are some common side effects:
- Bleeding from the operated site
- Seepage from the colonic edge, especially at the juncture from where it was ligatured and removed
- Clotting of the blood vessels in the deeper venous layer and the clots getting transported to the lungs causing pulmonary embolism which could turn fatal
- Increased likelihood of the urinary bladder, ureter, large and small intestines suffering injury
- Heightened risk of infection
Precautions
 Once you’re through with the surgery, you’ll need to abide by the surgeon’s instructions to stay safe and secure. Your surgeon will generally list the following instructions and precautions:
Once you’re through with the surgery, you’ll need to abide by the surgeon’s instructions to stay safe and secure. Your surgeon will generally list the following instructions and precautions:
- Walking from the day following the surgery to minimize chances of muscle soreness and blood clots
- Taking the prescribed medications on time and completing the medicine course
- Cleaning the incisions regularly to prevent infection risks
- Watching out for symptoms of infection diarrhea, abdominal cramps, and inflammation in the incisions and reporting the same to your physician immediately
Prognosis
Most patients convalesce from appendicitis within 4-5 weeks of the conduction of laparoscopic appendectomy. Nevertheless, a very slim chance of getting infected is always present.
Concluding Remarks
Laparoscopic appendectomy is generally resorted to when there is imminent risk of the inflamed appendix bursting open. The risks related to leaving appendicitis untreated are remarkably grave and could endanger the affected individual’s life. For complete information on laparoscopic appendix surgery of the appendix, you can contact our general surgeon and make an appointment with him for possible surgery.
References
- https://www.sages.org/publications/patient-information/patient-information-for-laparoscopic-appendectomy-from-sages/
- https://www.healthline.com/health/appendectomy#recovery
- https://www.hopkinsmedicine.org/healthlibrary/test_procedures/gastroenterology/appendectomy_92,P07686
- https://www.everydayhealth.com/appendicitis/guide/appendectomy/
- https://www.findatopdoc.com/Healthy-Living/Everything-You-Need-to-Know-About-an-Appendectomy
- https://www.cochrane.org/CD006437/COLOCA_determining-optimal-method-securely-closing-base-appendix-during-keyhole-surgery-after-removal
- https://www.healthpages.org/surgical-care/what-kind-surgeon/
- https://www.cochrane.org/CD006437/COLOCA_determining-optimal-method-securely-closing-base-appendix-during-keyhole-surgery-after-removal
Surgery for Esophageal Cancer – General Surgeon NYC
Esophagus Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
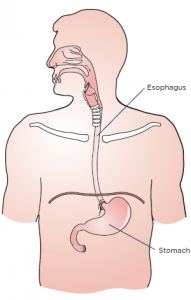
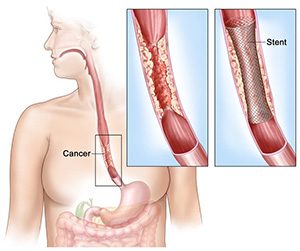
Esophagogastrectomy or esophagus surgery entails doing away with the entire esophagus (and often a stomach part) for treating esophageal cancer, Barrett’s esophagus, achalasia, esophageal stenosis, and GERD. The thoracic surgeon transforms the remaining section of the stomach into a tubular form serving as the replacement for the excised esophagus. The reconstructed esophagus enables the patient to swallow as he or she was doing before the surgery.
Steps
A surgical team comprising of medical specialists and headed by a thoracic or general surgeon performs esophagogastrectomy. The surgical procedure is usually open-type and is carried out in three separate ways.
- Transthoracic esophagectomy (TTE) is conducted via the chest cavity
- Transmittal esophagectomy (THE) is performed by making incisions in the breastbone and the neck’s left side
- En bloc esophagectomy is performed by perforating the abdomen, chest, and neck
Nowadays, the majority of the esophageal surgeries are done using the minimally-invasive laparoscopic procedure where 5-6 fine incisions are made in the abdomen, chest, and neck. The total number of slits (along with their locations) to be made are decided based on the purpose of carrying out the operation and whether the patient has undergone abdominal or thoracic surgeries on previous occasions.
Regardless of the type or method used, the operation is complex thereby necessitating an extended stay in the hospital. If the metastasis is limited to the esophagus and not spread further, excising the gullet and adjacent lymph nodes might help reverse cancer. Alas, most of the cases are detected at an advanced stage compelling the surgeon to go for a compound surgery.
Benefits
Minimally invasive esophagectomy has proven to be more effective compared to open esophagectomy as the postoperative mortality and morbidity rates related to the former are much lower. There are numerous studies to corroborate the outcomes associated with MIE are better than PE. Some of the likely benefits associated with MIE vis-à-vis PE comprise:
- Ashorter period of hospitalization
- Less painful procedure
- Reduced risk of complications or infections
- Less bleeding (and hence fewer transfusions)
- Speedier return to leading a normal life
Side Effects
Some complications related to esophageal surgery are common to other forms of surgery including but not limited to:
- Stroke and heart attack (while the operation is in progress)
- Shortness of breath
- Anastomotic leaking (low blood pressure, vomiting, surgical wound drainage, increased heart rate, and so on)
- Bleeding
- Pulmonary embolism
Complications or risks particularly associated with esophagogastrectomy (which are somewhat rare) include:
- Acute chest infection
- Pulmonary complications, particularly pneumonia
- An injury or wound to the adjacent organs during the operation
- Leakage at the junction of the conjoined stomach and esophagus
Precautions
The surgeon who will operate will spell out the risks about the surgery as well as the preparations and precautions you to need to take before, after and during the procedure. You’ll have to quit smoking altogether at least before the surgery and possibly afterward as well. You’ll have to abide by the instructions specified by your surgeon once you’re discharged from the hospital.
The precautions that you’ll need to take will revolve around your diets, medications, clothing, personal accessories, and lifestyle.
Prognosis
The quality of life of most patients improves post-surgery, but some complications linger on. Follow-up care in the form of pain management, lung therapy, psychosocial care, and nutritional evaluations are highly recommended by the medic to keep the complications or risks at bay.
Concluding Remarks
Minimally invasive esophagectomy or esophagogastrectomy is evidentially the best form of surgical treatment for patients with esophageal cancer. If you or somebody close to you has been diagnosed with neoplasm of the esophagus, you can contact us to make an appointment with our general surgeon for a consultation.
References
- https://www.uwhealth.org/healthfacts/surgery/4281.pdf
- https://www.cancer.org/cancer/esophagus-cancer/treating/surgery.html
- https://www.ariahealth.org/programs-and-services/surgery/general-surgery/surgery-for-esophagus
- https://www.cancercenter.com/esophageal-cancer/surgery/
- https://www.healthline.com/health/esophagectomy-open#postsurgery
- https://www.cancercenter.com/esophageal-cancer/da-vinci-surgical-system/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4283863/
- https://www.mayoclinic.org/tests-procedures/esophagectomy/about/pac-20385084
- https://www.uwhealth.org/healthfacts/surgery/4281.pdf
- https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=134&contentid=154