CALL TODAY 646-846-1136 | EMAIL
Surgical Experts Dedicated to Improving Lives
At Lenox Hill Surgeons, our dedicated team of nyc surgeons and medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments.We specialize in general surgery, including extensive experience in performing hernia repair surgery. Our expertise is in minimally invasive surgery and robotic surgery. Minimally invasive and robotic surgery often allow patients to experience easier recovery than traditional open surgery. They also allow for more precise and less traumatic surgery. When robotic and minimally invasive surgery is not an option, we are also skilled and experienced in traditional open surgical procedures.
All of our doctors are experienced and skilled surgeons having undergone extensive training in school, residency and fellowships. They all practice medicine with ethical behavior, compassion and superb bedside manner. In the operating room they all exhibit precise mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These innate and learned skills allow our surgeons to be some of the most dexterous and skilled professionals in all of New York City and the Country.
Call us: 646-846-1136
About The Surgeons
PATIENT TESTIMONIALS
Recent Awards
We are honored and deeply appreciative to have consistently received prestigious awards and recognition year after year, establishing us as one of New York’s foremost hospitals for a wide range of general surgeries, safety measures, specialized procedures, and overall excellence in healthcare. At Lenox Hill Surgeons, our unwavering commitment lies in delivering exceptional care and unwavering support to our patients, guaranteeing their safety and successful recovery throughout their entire surgical experience.
Hospital Quality Awards
 America’s 50 Best Hospitals Award™ (2023, 2022)
America’s 50 Best Hospitals Award™ (2023, 2022)
Top 1% in the nation for providing the highest clinical quality year over year.

America’s 100 Best Hospitals Award™ (2021)
Top 2% in the nation for consistently delivering clinical quality year over year.

America’s 250 Best Hospitals Award™ (2023, 2022, 2021)
Top 5% in the nation for consistently delivering clinical quality.

Patient Safety Excellence Award™ (2023, 2022)
Top in the nation for providing excellence in patient safety by preventing infections, medical errors, and other preventable complications.
Specialty Clinical Quality Awards

America’s 100 Best Hospitals for Cardiac Care Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in heart bypass surgery, coronary interventional procedures, heart attack treatment, heart failure treatment, and heart valve surgery.

America’s 100 Best Hospitals for Coronary Intervention Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in coronary intervention procedures (angioplasty with stent).

America’s 100 Best Hospitals for Prostate Surgery Award™ (2023, 2022, 2021)
Superior clinical outcomes in prostate removal surgery and transurethral resection of the prostate.
Click to see all of our Healthgrades best doctors awards


Visit our main website at www.LenoxHillSurgeons.com
Blog Posts are Below:
Author Archives: L65auzT3
Gallbladder and Gallstone Surgery – NYC General Surgeon
Gallstone and Gallbladder Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
 Gallstone and gallbladder surgery referred to as cholecystectomy in medical parlance, is an operative procedure where your gallbladder is removed. Gallbladder surgery is chiefly performed to get rid of gallstones or cholesterol stones which if not removed could lead to severe complications like cholangitis, pancreatitis, and cholecystitis. Gallbladder deletion or excision is the best solution if this biliary-tract organ becomes swollen (cholecystitis) or infected or if you’re diagnosed with biliary dyskinesia (compromised outflow of bile), choledocholithiasis or pancreatitis.
Gallstone and gallbladder surgery referred to as cholecystectomy in medical parlance, is an operative procedure where your gallbladder is removed. Gallbladder surgery is chiefly performed to get rid of gallstones or cholesterol stones which if not removed could lead to severe complications like cholangitis, pancreatitis, and cholecystitis. Gallbladder deletion or excision is the best solution if this biliary-tract organ becomes swollen (cholecystitis) or infected or if you’re diagnosed with biliary dyskinesia (compromised outflow of bile), choledocholithiasis or pancreatitis.
Cholecystectomy is the most popular and preferred treatment mode of doing away with gallstones as these do not resolve or dissolve as a matter of course. You know that you’re due for surgery when you suffer from acute abdominal pain, nausea, vomiting, flatulence, fever or jaundice.
Surgery Types & Methods
In very rare circumstances, gallstones can be melted away or resolved by making dietary changes like reducing consumption of fatty foods or taking certain medications. However, these strategies are, for the most part, ineffective if the stones are sizable. For nearly 80% of individuals with gallstones, surgery is the best and the only alternative.

There are primarily three surgical procedures that surgeons carry out for gallstone elimination: cholecystectomy (gallbladder resection), ERCP (endoscopic retrograde cholangiopancreatography), and cholecystostomy (drainage of the bladder).
- Cholecystectomy is the most widely used technique for clearing away cholesterol stones. Two types of gallbladder surgery are in vogue-laparoscopy (keyhole surgery) and open surgery. The laparoscopic operation is more popular in comparison to the open surgery mode because of the former’s inherent benefits.
- The open surgical method is resorted to especially when anatomical issues are resulting from previous gastrointestinal surgeries, like the presence of scar tissues. Though it takes roughly 1-2 hours for performing both the types of operation, open surgery entails a longer stay in the hospital and an extended recovery period, largely because of the wider opening.
- In ERCP, an endoscope is inserted into the small intestine via the esophagus for dealing with an obstructed common bile duct. Surgical tools are slotted in together with the endoscope for correcting the constricted or blocked sections of CBD once the gallbladder is excised. Often, it may not be possible to conduct surgery on some patients.
In these circumstances, the excess bile is drained away from the bladder with the help of a catheter. Nevertheless, these patients will have to consider surgery in the long run.
Benefits
Opting for a laparoscopic or open gallbladder surgery has its benefits. Removing a diseased or contaminated bladder ensures that you’ll be able to get back to leading a normal life quickly. Choosing laparoscopic intervention ascertains that your hospital stay will be shorter-you may be discharged on the very day the operation is performed. Also, the recuperation will be faster compared to open surgery.
The chances of the complications returning or recurring are also very slim once the surgery is done.
Side Effects
- Bleeding
- A hernia
- Blood clots
- Heart attack or stroke
- Wound infection
- Abdominal swelling
- Allergic reactions from general anesthesia
- Bile leakage
- Pneumonia
- The possibility of damage to organs surrounding the gallbladder
Precautions
- Cleanse and dress the incision area periodically
- Walk as much as you can to prevent thrombosis
- Wear loose fitting clothes so that the incision is not abraded against
- Follow the dietary chart prescribed by the surgeon
- Take all medications on time and complete the course
Prognosis
 As far as the short-term prognosis is concerned, the success rate of bladder operations is excellent. The kind of surgery you go for determines the recuperation period. You’ll experience mild postoperative pain if laparoscopy is involved. Talking about the long-term scenario, you’re less likely to suffer from the complications you had before the surgery.
As far as the short-term prognosis is concerned, the success rate of bladder operations is excellent. The kind of surgery you go for determines the recuperation period. You’ll experience mild postoperative pain if laparoscopy is involved. Talking about the long-term scenario, you’re less likely to suffer from the complications you had before the surgery.
Concluding Remarks
Laparoscopic or open surgery is the feasible option for getting relief from complications or issues related to the gallbladder. For more details about this treatment option and to evaluate if this is the right stage to get this treatment, we advise you to fix an appointment with one of our specialists for consultation.
References
- https://www.hon.ch/HONselect/Selection/E04.html
- https://www.healthline.com/health/gallbladder-removal-open#outlook
- https://www.healthline.com/health/gallbladder-removal-laparoscopic#follow–up
- https://www.uofmhealth.org/health-library/hw106860
- https://www.webmd.com/digestive-disorders/surgery-for-gallstones#1
- https://www.sages.org/publications/patient-information/patient-information-for-laparoscopic-gallbladder-removal-cholecystectomy-from-sages/
- https://www.everydayhealth.com/gallbladder/surgery-what-expect/
Spleen Surgery – NYC General Surgeon
Spleen Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
Surgical excision of the spleen or splenectomy becomes imperative when this vital immunologic organ becomes diseased or cancerous or is damaged due to an injury or wound. You could also be a potential candidate of splenectomy if you suffer from an acute blood disorder (polycythemia vera, idiopathic thrombocytopenic purpura, hemolytic anemia or sickle cell anemia) or have a ruptured or enlarged spleen resulting from trauma. Since the spleen is a vital cog in the immunity system, helping to combat diseases and removing worn-out and damaged cells from the bloodstream, its absence could leave you vulnerable to infections.
As removal of the spleen compromises the healthy functioning of your immunological system, you’ll need to take prophylactic antibiotics and vaccines on a regular basis.
Steps
A spleen operation is either performed as an open surgery mode or laparoscopically. In open surgery, the surgeon makes a long and broad cut across the left side of the abdomen, and after that excises the spleen. The opening is then ligatured using sterilized catgut. Open splenectomy is suitable for patients with a swollen or ruptured spleen; those with disfigured splenic tissues from past surgeries, and those who are overweight.
The procedure for laparoscopic splenectomy is nearly the same as the traditional technique only that the former is more advanced. This surgical technique entails the insertion of a laparoscope via a few tiny cuts or keyhole incisions made in the abdomen. A high-resolution video camera attached at the laparoscope’s head transmits images of the spleen and the surrounding area to a large VDU.
The surgeon based on the transmitted images channels small surgical tools inside the highlighted area for cutting off the spleen. The incisions are then sewn up.
Benefits
Splenectomy is usually the last resort to get rid of an infected or dysfunctional spleen. As the surgery can considerably weaken the immune system, the operation should be carried out only on an emergency basis. Nevertheless, a spleen surgery can help mitigate a range of health problems including but not limited to benign or malignant cysts, infection, and blood disorders that may not be treatable through other techniques.
Side effects
The risks or complications about a splenectomy usually involve:
- Bleeding from the operated area
- Infection
- Heart attack or stroke
- Thrombosis or blood clots
- Allergic reactions resulting from general anesthesia
- Breathing problems
- Pus formation beneath the diaphragm
- Pneumothorax or lung collapse
- Herniation in the incision area
- Venous blood clot shifting to the liver causing portal vein thrombosis
- Organs in the vicinity of the spleen like stomach, pancreas, and gallbladder becoming dysfunctional
Precautions
 Before the surgery, you’ll be recommended to stop taking specific medicinal supplements and medicines. At the same time, you may have to refrain from consuming foods and water. You also may have to go for blood transfusion, (depending on the state of your health) to make sure that you do not become deficient in blood after the operation. You’ll be inoculated with a pneumococcal vaccine to minimize risks of infection once your spleen is expunged.
Before the surgery, you’ll be recommended to stop taking specific medicinal supplements and medicines. At the same time, you may have to refrain from consuming foods and water. You also may have to go for blood transfusion, (depending on the state of your health) to make sure that you do not become deficient in blood after the operation. You’ll be inoculated with a pneumococcal vaccine to minimize risks of infection once your spleen is expunged.
Prognosis
You’ll stay in the hospital for about a week following the surgery and depend upon the severity of the complication; complete convalescence might take 5-7 weeks. In the long term, you’ll tend to stay healthy but will remain vulnerable to particular infections and to alleviate the chances of outbreak you’ll have to take prophylactic antibiotics and inoculations lifelong. For more details on how Spleen surgery can be beneficial for you, you can consult our specialists by making an appointment.
References
- https://www.jstor.org/stable/3406279?seq=1#page_scan_tab_contents
- https://www.healthline.com/health/spleen-removal#outlook
- https://www.webmd.com/digestive-disorders/splenectomy#1
- https://www.mayoclinic.org/tests-procedures/splenectomy/about/pac-20395066
- https://www.sages.org/publications/patient-information/patient-information-for-laparoscopic-spleen-removal-splenectomy-from-sages/
- https://my.clevelandclinic.org/health/treatments/14614-splenectomy
- https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=zc2195
Pancreas Surgery – NYC General Surgeon
Pancreas Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
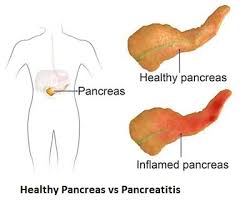
 The pancreas being a key organ of the endocrine and digestive systems of the body is indispensable for the smooth functioning of the human body. Hence, a diseased condition of the pancreas, like a tumor, abscess or malignancy that causes pancreatitis and makes the dysfunctional organ calls for pancreatic surgery. There are different methods, or kinds of pancreas surgery and the type that a patient will have to opt for will depend upon whether his or her pancreatitis is chronic or acute.
The pancreas being a key organ of the endocrine and digestive systems of the body is indispensable for the smooth functioning of the human body. Hence, a diseased condition of the pancreas, like a tumor, abscess or malignancy that causes pancreatitis and makes the dysfunctional organ calls for pancreatic surgery. There are different methods, or kinds of pancreas surgery and the type that a patient will have to opt for will depend upon whether his or her pancreatitis is chronic or acute.
More often than not, the condition or syndrome can be treated and managed without going for invasive intervention or surgery. Nevertheless, if an infection or degeneration of the pancreatic tissues becomes longstanding and acute, surgery is the only treatment option.
Steps
 The most common pancreatic surgery procedures include minimally invasive pancreatic resection, spleen-preserving pancreatectomy, ‘The Whipple’, and Enucleation of pancreatic tumor.’ Minimally invasive pancreatic resection surgery is conducted laparoscopically giving the interventional radiologist or gastroenterologist good access to the abdomen via tiny keyhole notches. This surgical method is appropriate for patients having pancreatic cysts.
The most common pancreatic surgery procedures include minimally invasive pancreatic resection, spleen-preserving pancreatectomy, ‘The Whipple’, and Enucleation of pancreatic tumor.’ Minimally invasive pancreatic resection surgery is conducted laparoscopically giving the interventional radiologist or gastroenterologist good access to the abdomen via tiny keyhole notches. This surgical method is appropriate for patients having pancreatic cysts.
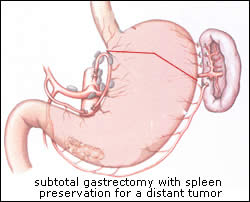
Spleen-preserving pancreatectomy is conducted laparoscopically where the pancreas is excised, but the spleen is kept intact for preserving its immunological functionality as well as minimize the risks of complications and infections in the future. The traditional pancreatectomy method entails the removal of the spleen along with the metastatic pancreas for reversing the spread of cancer. Nevertheless, if the surgery is carried out for a benign condition like pancreatic tumor or cyst, then spleen resection is not necessary.
Enucleation process is appropriate for dealing with benign or non-cancerous tumors where these are scraped out carefully instead of expurgating a large pancreatic section.
‘The Whipple’ surgery or ‘pancreaticoduodenectomy’ is the go-to procedure for treating pancreatic cancer and also for dealing with complications or abscesses related to the bile duct, intestine, and pancreas. The surgery where the top of the pancreas, bile duct, gallbladder, and duodenum are removed can be extremely complex and demanding, fraught with risks.
Benefits
If the surgery is for treating pancreatitis or tumors, then opting for laparoscopic surgery is the best option. In such a case, recuperation is faster necessitating a shorter hospital stay. However, if the surgery is for pancreatic cancer, then the operation lasts for several hours and the patient may have to be in the hospice for at least a week.
Complete recovery might take many weeks and even months. Benefits of going for a major pancreatic surgery are:-
- Best treatment technique for remedying cancer and reversing chronic pancreatitis
- Increased lifespan
- Digestive issues and complications associated with pancreas might be resolved post surgery
- Chemotherapy and radiotherapy for continued treatment in case cancer recurs
Side Effects
Pancreatic surgeries for dealing with cancer tend to be extremely complicated, and it is no wonder that such operations have a very high mortality rate. Nearly 50% of the patients report grave complications and about 2%-4% expire. The most common risks include:-
- Wound infection or cardiac infection
- Hemorrhage (bleeding)
- Leakage from pancreas from the point where it is linked with the intestine
- Allergic reaction to general anesthesia (very rare)
Precautions
Fully recuperating from a complex pancreas surgery takes time and the convalescing process could be exhausting, especially for older patients. You’ll be required to report to your surgeon 1-2 times in a month following your recovery. The doctor will evaluate your progress and may recommend CT or MRI scans, and blood tests to ensure that there is no recurrence of cancerous tumors or lesions.
Dietary and lifestyle changes to have to be made to maintain overall health and also to reduce the risks of relapse.
Prognosis
Pancreatic cancer and all other serious complications of the pancreas are, by and large, regarded as untreatable and hence incurable. Nevertheless, the mortality rates related to pancreatic cancer (post surgery) have steadily declined over the decades.
Concluding Remarks
Living without a pancreas can be a challenge for any individual. If you’re diagnosed with a tumor or inflammation of your pancreas, you can continue to live an almost normal life, provided you opt for an appropriate treatment plan and abide by our physician’s guidelines. If you’ve cancer, then surgical removal of the pancreas is the only option. However, you’ll have to keep your fingers crossed on whether cancer will recur or not.
References
- https://www.mayoclinic.org/tests-procedures/whipple-procedure/about/pac-20385054
- https://stanfordhealthcare.org/medical-treatments/c/cancer-surgery/types/complex-pancreatic-surgery.html
- https://www.mskcc.org/blog/drug-reduces-risk-serious-pancreatic-surgery-complication
- https://stanfordhealthcare.org/medical-treatments/p/pancreatic-surgery/types/spleen-preserving-pancreatectomy.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2023932/
- https://www.ariahealth.org/programs-and-services/surgery/general-surgery/pancreatic-surgery
- http://columbiasurgery.org/pancreas/what-expect-after-operation
- https://www.cancer.org/cancer/pancreatic-cancer/treating/surgery.html
- http://pancreatic.org/pancreatic-cancer/about-the-pancreas/prognosis/
What to do after Stomach Surgery
What You Need to Do After Stomach Surgery
There are various different types of stomach surgery that can be performed for a range of different reasons. By and large, this type of surgery will be a major one, which means that you will need to be prepared for a lengthy recovery period and you need to know the ins and outs of what you should be doing once you have had the surgery.
Important factors to bear in mind
When you have stomach surgery, there are a number of important factors that you need to bear in mind. First off, make sure you plan ahead and arrange for someone to come and collect you from the hospital on the day of discharge. You won’t be able to drive home on your own or walk/use public transport after a major surgery, so ensure you have someone on hand to help.
Once home following the surgery, it is a good idea to have someone come and stay for a while – perhaps a few days or a week just in case there are any issues. If you live alone, arrange this in advance so that you have minimal stress to deal with once the surgery is over. In addition, you will need to get plenty of rest so you need to have someone around to do day to day tasks for you while you take it easy.
Before you leave the hospital, you will most likely receive details about what you should and shouldn’t eat after your stomach surgery. Make sure you familiarize yourself with this and check with a professional if there is something you are not sure on. The food in these plans is designed to ensure you get the vitamins and minerals you need without causing any issues, so you need to follow it.
 One more thing that may be beneficial depending on the type of stomach surgery you have had is an abdominal binder. This provides valuable support while you are going through the recovery period, so it may be worth speaking to your doctor to see whether it is something that could help you and boost your recovery.
One more thing that may be beneficial depending on the type of stomach surgery you have had is an abdominal binder. This provides valuable support while you are going through the recovery period, so it may be worth speaking to your doctor to see whether it is something that could help you and boost your recovery.
Do bear in mind that there are generally a variety of side effects that come with stomach surgery, so you need to prepare yourself for this. Your doctor will be able to provide further information based on the surgery and your general health.
Seek advice from an expert
To learn more about recovering after major stomach surgery, you can get in touch with one of the best general surgeons in NYC for advice and information.
Hernia Repair Surgery – NYC Surgeon
Hernia Repair Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
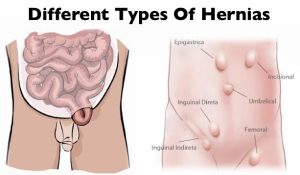 Hernia repair surgery entails the application of instrumental and manual procedures for correcting herniation of tissues or viscera including groin, abdomen, brain, and diaphragm. Internal organs, composed of tissues, could get herniated or bulged, forcing them to protrude via the wall encasing them. Hernias involving the groin (an inguinal hernia) and the umbilical cord (an umbilical hernia) are two of the most prevalent forms of a hernia.
Hernia repair surgery entails the application of instrumental and manual procedures for correcting herniation of tissues or viscera including groin, abdomen, brain, and diaphragm. Internal organs, composed of tissues, could get herniated or bulged, forcing them to protrude via the wall encasing them. Hernias involving the groin (an inguinal hernia) and the umbilical cord (an umbilical hernia) are two of the most prevalent forms of a hernia.
Since a hernia does not heal on its own but rather expands over time, it is crucial that you opt for surgical treatment to avoid unnecessary/preventable complications in the long run. Hernia surgery, usually performed on an outpatient basis, is a moderately simple operation that can help remedy the organ’s bulging and restore it to its original position.
Steps
 Two of the most popular types of hernia repair surgery is ‘herniorrhaphy’ and ‘hernioplasty’. Herniorrhaphy-the traditional hernia repair technique-is still conducted extensively where the surgeon makes a wide and long notch over the herniated organ. Thereafter, the physician removes the protrusion and reinstates the dislodged organ or tissues to its actual site.
Two of the most popular types of hernia repair surgery is ‘herniorrhaphy’ and ‘hernioplasty’. Herniorrhaphy-the traditional hernia repair technique-is still conducted extensively where the surgeon makes a wide and long notch over the herniated organ. Thereafter, the physician removes the protrusion and reinstates the dislodged organ or tissues to its actual site.
Finally, the doctor sutures the hole in the muscle via which the protuberance developed, sterilizes the incision, and sews it up. Hernioplasty is very much similar to herniorrhaphy procedurally excepting that in the final step, the surgeon overlays a sterile mesh (produced from animal tissues or polypropylene) on the muscular notch rather than suturing it. The nature or type of your herniation will determine the mode of repair surgery you’ll need to opt for.
Strangulated, reducible, and irreducible hernias are the three most widespread kinds of hernias. Both of the aforementioned surgical operation procedures can be carried out using a laparoscope or via open surgery.
Benefits
Both hernioplasty and herniorrhaphy are straightforward and uncomplicated surgical repair processes that take about 30-40 minutes to complete. You won’t feel any pain as the surgery will be done using either local or general anesthesia. Majority of patients are discharged from the hospital or medical center on the very day the laparoscopic surgery is performed. The usual benefits of the laparoscopic repair operation include:-
- Very short duration of stay
- Faster healing
- Reduced pain post surgery
- Quicker return to normal life
- Minimal costs (including all the expense heads)
- Lower risks of infection
Side Effects
The side effects of this type of surgery, most of which are rare, involve:-
- Swelling and redness around the incision or opening
- Blood clot
- Mesh pain
- Urinary tract infection
- Urinary incontinence
- Infection
- Difficulty urinating
- Hernia recurrence
- Neuralgia or nerve damage
- Constipation
- Kidney failure or complications
- Breathing problems or pneumonia
Precautions
You must abide by the surgeon’s instructions once you return home (which are usually on the same day the surgery is carried out) for a speedy recovery. Take all the prescribed medications on time, including the anti-inflammatory drugs for minimizing the possibilities of incision swelling. Contact your surgeon instantly if you’ve recurrent spells of fever, coughs, chills, nausea, abdominal swelling, bleeding as well as experience difficulty in urinating. Make sure you get sufficient rest for at least two weeks following the operation so that you can get back to work at the earliest.
Prognosis
Most hernia surgeries are effective, enabling patients to recover fully within 4-6 weeks. A typical person who has undergone hernia repair surgery can resume normal activities 2 weeks after the procedure.
Concluding Remarks
Opting for a surgical procedure for remedying a hernia is highly recommended not only for avoiding complications which could take a fatal turn (though very rare) but also for going back to leading a normal life. You can make an appointment with our general surgeon for a detailed, one-to-one consultation.
References
- http://www.medtronic.com/us-en/patients/treatments-therapies/hernia-surgery/about-recovery.html
- https://www.webmd.com/digestive-disorders/inguinal-hernia#1
- https://www.medicalnewstoday.com/articles/319753.php
- https://www.highgatehospital.co.uk/things-you-need-to-know-hernia-operation/
- https://www.webmd.com/digestive-disorders/need-surgery-hernia#1
- http://columbiasurgery.org/news/2014/04/15/hernias-what-you-need-know
- https://en.wikipedia.org/wiki/Hernia_repair
- https://my.clevelandclinic.org/health/treatments/6905-laparoscopic-surgery-for-hernia-repair/risks–benefits
Laparoscopic appendectomy – NYC General Surgeon
Laparoscopic appendectomy: Steps, Benefits, Side-Effects, Precautions & Prognosis
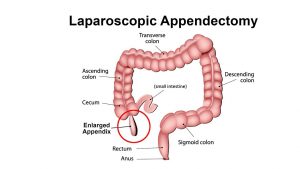
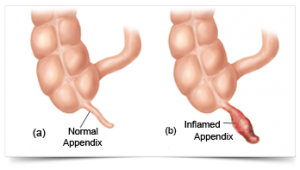
 The procedure of surgically removing the narrow, elongated tube attached to the colon-known as an appendix when it becomes diseased, inflamed or infected (appendicitis) is called appendectomy. It is normally carried out on an emergency basis as swollen appendicitis could burst if not excised, causing the clogged stool and bacteria to spread. It would eventually infect other gastrointestinal organs and lead to peritonitis-a life-threatening condition. A ruptured appendix could also create an abdominal abscess which is also a grave condition that could endanger your life.
The procedure of surgically removing the narrow, elongated tube attached to the colon-known as an appendix when it becomes diseased, inflamed or infected (appendicitis) is called appendectomy. It is normally carried out on an emergency basis as swollen appendicitis could burst if not excised, causing the clogged stool and bacteria to spread. It would eventually infect other gastrointestinal organs and lead to peritonitis-a life-threatening condition. A ruptured appendix could also create an abdominal abscess which is also a grave condition that could endanger your life.
Steps
Generally, two kinds of appendectomy are carried out to do away with appendicitis:
- The traditional ‘open appendectomy’
- Laparoscopic appendectomy (a more advanced form of surgery)
 Open appendectomy is more suitable for patients whose appendices have split open and also for those who have undergone abdominal surgery before.
Open appendectomy is more suitable for patients whose appendices have split open and also for those who have undergone abdominal surgery before.
A laparoscopic appendectomy, on the other hand, involves accessing the appendix via three tiny incisions or openings made in the lower abdomen. A cannula filled with carbon dioxide (a slender and small tube) is inserted through the openings for inflating the abdomen following which a laparoscope is slotted in.
A high-resolution camera fixed at the head of the laparoscope transmits the image to a display screen. The displayed images will clearly show the precise location of the appendix which in turn will help the surgeon to channelize the surgical instruments for ligation (of the appendix) and excising it. Keyhole surgery usually resorts if the patient happens to be overweight and aged.
Benefits
The specific benefits of laparoscopic appendectomy vary from one patient to another, depending upon his or her condition. Nevertheless, the common benefits entail:
- Short stay in the hospital
- Reduced postoperative pain
- Faster restoration of normal bowel function
- Speedier return to a normal lifestyle
Side Effects
The associated risk factors or complications are more or less the same for both laparoscopic appendectomy and open appendectomy. Following are some common side effects:
- Bleeding from the operated site
- Seepage from the colonic edge, especially at the juncture from where it was ligatured and removed
- Clotting of the blood vessels in the deeper venous layer and the clots getting transported to the lungs causing pulmonary embolism which could turn fatal
- Increased likelihood of the urinary bladder, ureter, large and small intestines suffering injury
- Heightened risk of infection
Precautions
 Once you’re through with the surgery, you’ll need to abide by the surgeon’s instructions to stay safe and secure. Your surgeon will generally list the following instructions and precautions:
Once you’re through with the surgery, you’ll need to abide by the surgeon’s instructions to stay safe and secure. Your surgeon will generally list the following instructions and precautions:
- Walking from the day following the surgery to minimize chances of muscle soreness and blood clots
- Taking the prescribed medications on time and completing the medicine course
- Cleaning the incisions regularly to prevent infection risks
- Watching out for symptoms of infection diarrhea, abdominal cramps, and inflammation in the incisions and reporting the same to your physician immediately
Prognosis
Most patients convalesce from appendicitis within 4-5 weeks of the conduction of laparoscopic appendectomy. Nevertheless, a very slim chance of getting infected is always present.
Concluding Remarks
Laparoscopic appendectomy is generally resorted to when there is imminent risk of the inflamed appendix bursting open. The risks related to leaving appendicitis untreated are remarkably grave and could endanger the affected individual’s life. For complete information on laparoscopic appendix surgery of the appendix, you can contact our general surgeon and make an appointment with him for possible surgery.
References
- https://www.sages.org/publications/patient-information/patient-information-for-laparoscopic-appendectomy-from-sages/
- https://www.healthline.com/health/appendectomy#recovery
- https://www.hopkinsmedicine.org/healthlibrary/test_procedures/gastroenterology/appendectomy_92,P07686
- https://www.everydayhealth.com/appendicitis/guide/appendectomy/
- https://www.findatopdoc.com/Healthy-Living/Everything-You-Need-to-Know-About-an-Appendectomy
- https://www.cochrane.org/CD006437/COLOCA_determining-optimal-method-securely-closing-base-appendix-during-keyhole-surgery-after-removal
- https://www.healthpages.org/surgical-care/what-kind-surgeon/
- https://www.cochrane.org/CD006437/COLOCA_determining-optimal-method-securely-closing-base-appendix-during-keyhole-surgery-after-removal
Surgery for Esophageal Cancer – General Surgeon NYC
Esophagus Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
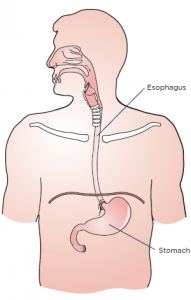
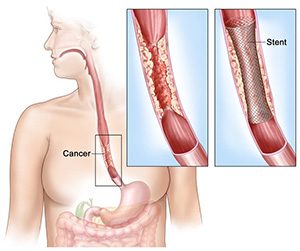
Esophagogastrectomy or esophagus surgery entails doing away with the entire esophagus (and often a stomach part) for treating esophageal cancer, Barrett’s esophagus, achalasia, esophageal stenosis, and GERD. The thoracic surgeon transforms the remaining section of the stomach into a tubular form serving as the replacement for the excised esophagus. The reconstructed esophagus enables the patient to swallow as he or she was doing before the surgery.
Steps
A surgical team comprising of medical specialists and headed by a thoracic or general surgeon performs esophagogastrectomy. The surgical procedure is usually open-type and is carried out in three separate ways.
- Transthoracic esophagectomy (TTE) is conducted via the chest cavity
- Transmittal esophagectomy (THE) is performed by making incisions in the breastbone and the neck’s left side
- En bloc esophagectomy is performed by perforating the abdomen, chest, and neck
Nowadays, the majority of the esophageal surgeries are done using the minimally-invasive laparoscopic procedure where 5-6 fine incisions are made in the abdomen, chest, and neck. The total number of slits (along with their locations) to be made are decided based on the purpose of carrying out the operation and whether the patient has undergone abdominal or thoracic surgeries on previous occasions.
Regardless of the type or method used, the operation is complex thereby necessitating an extended stay in the hospital. If the metastasis is limited to the esophagus and not spread further, excising the gullet and adjacent lymph nodes might help reverse cancer. Alas, most of the cases are detected at an advanced stage compelling the surgeon to go for a compound surgery.
Benefits
Minimally invasive esophagectomy has proven to be more effective compared to open esophagectomy as the postoperative mortality and morbidity rates related to the former are much lower. There are numerous studies to corroborate the outcomes associated with MIE are better than PE. Some of the likely benefits associated with MIE vis-à-vis PE comprise:
- Ashorter period of hospitalization
- Less painful procedure
- Reduced risk of complications or infections
- Less bleeding (and hence fewer transfusions)
- Speedier return to leading a normal life
Side Effects
Some complications related to esophageal surgery are common to other forms of surgery including but not limited to:
- Stroke and heart attack (while the operation is in progress)
- Shortness of breath
- Anastomotic leaking (low blood pressure, vomiting, surgical wound drainage, increased heart rate, and so on)
- Bleeding
- Pulmonary embolism
Complications or risks particularly associated with esophagogastrectomy (which are somewhat rare) include:
- Acute chest infection
- Pulmonary complications, particularly pneumonia
- An injury or wound to the adjacent organs during the operation
- Leakage at the junction of the conjoined stomach and esophagus
Precautions
The surgeon who will operate will spell out the risks about the surgery as well as the preparations and precautions you to need to take before, after and during the procedure. You’ll have to quit smoking altogether at least before the surgery and possibly afterward as well. You’ll have to abide by the instructions specified by your surgeon once you’re discharged from the hospital.
The precautions that you’ll need to take will revolve around your diets, medications, clothing, personal accessories, and lifestyle.
Prognosis
The quality of life of most patients improves post-surgery, but some complications linger on. Follow-up care in the form of pain management, lung therapy, psychosocial care, and nutritional evaluations are highly recommended by the medic to keep the complications or risks at bay.
Concluding Remarks
Minimally invasive esophagectomy or esophagogastrectomy is evidentially the best form of surgical treatment for patients with esophageal cancer. If you or somebody close to you has been diagnosed with neoplasm of the esophagus, you can contact us to make an appointment with our general surgeon for a consultation.
References
- https://www.uwhealth.org/healthfacts/surgery/4281.pdf
- https://www.cancer.org/cancer/esophagus-cancer/treating/surgery.html
- https://www.ariahealth.org/programs-and-services/surgery/general-surgery/surgery-for-esophagus
- https://www.cancercenter.com/esophageal-cancer/surgery/
- https://www.healthline.com/health/esophagectomy-open#postsurgery
- https://www.cancercenter.com/esophageal-cancer/da-vinci-surgical-system/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4283863/
- https://www.mayoclinic.org/tests-procedures/esophagectomy/about/pac-20385084
- https://www.uwhealth.org/healthfacts/surgery/4281.pdf
- https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=134&contentid=154
Stomach Surgery: Gastric Bypass by NYC Top Surgeon
Stomach Surgery (Gastric Bypass): Steps, Benefits, Side-Effects, Precautions & Prognosis
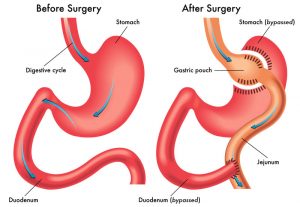
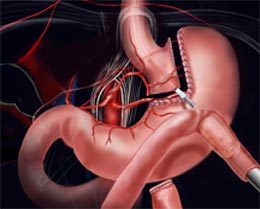
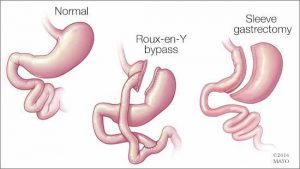 Gastric bypass is a type of surgical process chiefly carried out for treating a series of lifestyle conditions like type 2 diabetes, hypertension, obesity, and sleep apnea. These conditions more often than not occur concomitantly. The surgery is performed using a laparoscope (an elongated & slim tube featuring a high-resolution camera with intense light at the top) that is popped inside a slit made in the belly.
Gastric bypass is a type of surgical process chiefly carried out for treating a series of lifestyle conditions like type 2 diabetes, hypertension, obesity, and sleep apnea. These conditions more often than not occur concomitantly. The surgery is performed using a laparoscope (an elongated & slim tube featuring a high-resolution camera with intense light at the top) that is popped inside a slit made in the belly.
The laparoscope allows the surgeon to view the entire abdomen to restructure the small intestine to enable food to bypass the duodenum. This rearrangement leads to the body absorbing and assimilating fewer nutrients and calories, thereby enabling you to shed excess flab as well as stay fit and trim in the long run.
Steps
Stomach surgery is conducted in two distinct manners namely, open surgery and laparoscopy or laparoscopic surgery. In open surgery, the surgeon uses a scalpel for cutting open the stomach while in laparoscopy numerous small cuts are made in the abdomen. The end objective of both the types of surgery is to clearly view the digestive organs and the gastrointestinal tract and carry out the operation effectively.
The bypass surgery involves two necessary steps:
 1. The surgeon makes use of staples for sectioning the stomach into two halves: a larger bottom-half and a smaller upper half. The goal is to decrease the stomach’s size-the eventually reduced the volume of the upper section (known as pouch where the swallowed food will settle) will make you consume less, thereby letting you slim down.
1. The surgeon makes use of staples for sectioning the stomach into two halves: a larger bottom-half and a smaller upper half. The goal is to decrease the stomach’s size-the eventually reduced the volume of the upper section (known as pouch where the swallowed food will settle) will make you consume less, thereby letting you slim down.
2. The bypass surgery is performed in the 2nd step. The surgeon creates a notch in the pouch and links the jejunum (the initial part of the small intestine) with the opening. So, whatever you take will pass directly from the stomach’s upper pocket to the small intestine via this aperture, ultimately making you take in lesser calories.
On the whole, laparoscopy is preferred over general surgery as the former is less painful, involves shorter hospitalization and faster recuperation, and risks of infections are also lower.
Benefits
- The Roux-en-Y gastric bypass (the medical term for gastric surgery) results in considerable weight loss provided you fully abide by the instructions
- A good proportion of patients can maintain the postoperative bodyweight even 15-16 years after the surgery
- Optimal use of stored or available energy
- Feeling of fullness after taking a small meal and diminished appetite
Side effects
Like any other surgical procedure, gastric bypass is not without its complications and side effects. The following complications have been observed:
- Gastrointestinal/intra-abdominal hemorrhage
- Venous thromboembolism
- Increased risk of intra-abdominal infections like blisters and peritonitis
- Bowel obstruction
- A hernia
- Dumping of contents into the jejunum more frequently, especially when excessive foods or sugary foods are eaten
- Nutritional deficiencies (deficiency of calcium, iron, zinc, and folate as well as vitamins A, B1, and B12)
Precautions
There are certain precautions you’ll need to take once you’re released from the hospital following your surgery:
- Taking the prescribed medications on a regular basis
- Taking multivitamins, vitamin D, calcium, and vitamin B12 every day
- Taking balanced diets with limited consumption of calories
- Exercising daily for at least half an hour
- Remaining socially active
- Regular follow-up with the surgeon
Prognosis
Majority of individuals who opt for gastric surgery can lose 65% of their excess bodyweight. About 85% of those who undergo gastric bypass are successful in maintaining 50% of the excess weight they lost initially.
Concluding Remarks
Though gastric surgery is a practical solution for getting rid of inordinate bodyweight, the procedure can never be a panacea for obesity. If you wish to keep your weight under check post surgery and lead a fulfilling, healthy life, you’ll need to make lifestyle changes as well as heed dietary and exercise guidelines. To know more about stomach surgery as well as to fix an appointment with our bariatric surgeon, you can send us an email or contact us via phone.
References
- https://bariatric.surgery.ucsf.edu/conditions–procedures/laparoscopic-gastric-bypass.aspx
- https://medlineplus.gov/ency/article/007199.htm
- https://asmbs.org/patients/bariatric-surgery-procedures
- https://www.healthline.com/health/laparoscopy
- https://obesitynewstoday.com/gastric-bypass-success-rate/
- https://www.ucsfhealth.org/education/life_after_bariatric_surgery/
- https://www.acefitness.org/education-and-resources/lifestyle/blog/896/after-gastric-bypass-surgery-are-there-specific-exercise-precautions-i-should-take
Esophagus Surgery
What Happens After Esophagus Surgery?
The esophagus plays a vital part in our functioning, as it is the tube that enabled food to be moved from your throat when you swallow through to your stomach. This tube, which is around eight inches in length, is made up of muscles, which then contract to move food and drink along to your stomach.
Anyone that suffers from cancer of the esophagus or from severe damage of the stomach may find that they are in need of surgery. Either a section or the entire esophagus may need to be removed depending on the condition and the extent of the damage. In the event that the entire esophagus has to be removed, it is then rebuilt using sections of either the stomach or the large intestine.
What to expect
As you can imagine, this is a major surgery and the recovery period can be lengthy depending on the surgery carried out and any complications that may have arisen. You may need to spend a day or two in a high dependency ward immediately after the surgery, as this is a big operation. Being in this type of unit means that medics can keep a closer eye on you.
There will be a number of tubes in you when you come round for the surgery. These serve functions such as administering fluids, draining blood and fluid, draining the chest, and even checking on your blood pressure. In addition, once you start to come round properly and the anesthetic wears off, you will experience some pain and discomfort but will receive painkillers to help deal with this.
After a couple of days, you may be moved to a standard ward but you should expect to be in hospital for around ten days or so. After the surgery, you will have dressings applied to the wounds, and these will be changed after a couple of days and the wounds cleaned by medical staff. In addition, the clips or stitches that you have will stay in for around ten days and are generally removed prior to you leaving the hospital to go home. In the event you cannot have them taken out before being discharged, a nurse may come out to do this or you may have to return to hospital to have them removed.
Prior to your discharge, it is important that you pay careful attention to the information provided to you in relation to caring for your wounds while you heal.
Find out more from our expert
If you would like further information about esophagus surgery and would like to speak to an expert, get in touch with the best general surgeon in NYC today.
NYC General Surgeons Discuss Rheumatoid Arthritis
What is Rheumatoid Arthritis?

According to the Arthritis Foundation, there are approximately 1.5 million Americans who are living with rheumatoid arthritis right now. Both men and women can develop it, but statistics show that women are almost three times more likely to suffer from the condition. If you have recently been diagnosed with rheumatoid arthritis, or suspect you may have it, it’s imperative to learn all you can so you can find the best treatment plan for your specific needs.
Understanding Rheumatoid Arthritis

Classed as a chronic inflammatory autoimmune disorder, rheumatoid arthritis can severely affect a number of areas on a person’s body. While many people assume it just affects the joints, it doesn’t stop there. Rheumatoid arthritis can also affect a person’s heart, lungs, blood vessels, eyes, and even their skin. When a person has rheumatoid arthritis, their own body turns against itself and starts attacking the tissue.
Over time, it can cause swelling which is exceptionally painful, joint deformity, and even bone erosion.
What Are the Signs and Symptoms?

In the beginning stages of rheumatoid arthritis, typically the person may notice stiffness of the joints after activity or, in the morning, swollen joints, tender joints – joints that feel warm to the touch. Weight loss, fatigue, and even a fever are other common symptoms.
While each case is different, it tends to start in the fingers and toes; in other words, the smaller joints.
What Are the Causes?
While doctors understand how rheumatoid arthritis develops, what they are unclear about is what actually sets off that motion or process. When a body’s immune system starts to attack the synovium, then the process begins.
Some doctors believe that genes play a big factor in determining whether or not you will develop it, while others point towards environmental factors and even certain bacterial viruses.
What Are the Treatment Options?
 Because rheumatoid arthritis gets worse over time, leaving it is not an option. You want to get a proper diagnosis as early as possible, and then start up with an appropriate course of action. Treatment can include a medication such as NSAIDs and/or steroids, as well as physical therapy.
Because rheumatoid arthritis gets worse over time, leaving it is not an option. You want to get a proper diagnosis as early as possible, and then start up with an appropriate course of action. Treatment can include a medication such as NSAIDs and/or steroids, as well as physical therapy.
In severe or advanced cases, it may be necessary to have a surgeon repair or even rebuild the tissue that has been damaged. This will help to prevent more problems down the road.
Contact us today to schedule an appointment with the best surgeons in Manhattan.
Top General Surgeons in Manhattan – Carpal Tunnel Surgery
What is Carpal Tunnel Syndrome?

Have you been feeling numbness, tingling, or even itching sensation in your fingers or hand as of late? Does it feel like you don’t have the same strength in your fingers and hand as you used to? If so, you may be suffering from carpal tunnel syndrome. This particular condition affects women more often than men, but that’s not to say that men aren’t at risk.
Here’s a closer look at the condition including what it is, who is at risk, what the signs and symptoms are, and what you can do about treatment:
Understanding Carpal Tunnel Syndrome Better
 Carpal tunnel syndrome occurs when there is added pressure being placed on your median nerve. This nerve is found in your arm and actually runs all the way down your arm, right into your wrist. The area in which the nerve runs into is called the carpal tunnel, thereby giving this condition its name.
Carpal tunnel syndrome occurs when there is added pressure being placed on your median nerve. This nerve is found in your arm and actually runs all the way down your arm, right into your wrist. The area in which the nerve runs into is called the carpal tunnel, thereby giving this condition its name.
The median nerve is an important one in that it helps to control feeling in your thumb and movement in your first three fingers. When you have carpal tunnel syndrome, there is swelling in that passageway, which then restricts motion and can cause pain.
Unfortunately, it doesn’t go away on its own, and it will only continue to get worse over time if no treatment is taken.
What Are the Signs and Symptoms?
The typical signs and symptoms include numbness, itching, tingling, and burning in your thumb, fingers, or even the palm of your hand.
Who Is At Risk of Developing It?
As for who is most at risk of developing carpal tunnel syndrome, that would be people who engage in repetitive motions. It’s not uncommon for it to be related to work, such as a person who spends much of their workday typing or using machinery.
But those aren’t the only people at risk. Those who are pregnant, have rheumatoid arthritis, are obese, have diabetes, or who have hypothyroidism are also at high risk.

What Are the Treatments Available?
The treatment plan will depend on the individual and the severity of the condition. The first step is usually lifestyle changes, and from there medication may be prescribed. If this fails, then surgery can end up being necessary. Surgery may be needed to reconstruct and even repair tissue that has been damaged.
For more information, contact us today at 646-846-1136 to schedule an appointment with the best plastic surgeon in Manhattan.
What is a Phalangeal Fracture?
Your hands are one of those things you often take for granted, that is until you injure one and suddenly see how much you rely on them. Hand injuries can affect your ability to do your job, drive, and go about your daily life, not to mention they can cause a fair amount of pain and discomfort. One type of hand injury that can occur is a phalangeal fracture. While many of these types of injuries can just be treated with a simple splint, some cases aren’t so simple and may require surgery.
How Does a Phalangeal Fracture Happen?
 In order to understand how these fractures occur, it’s important to understand what the phalanges are. The phalanges are actually the bones in your fingers, but they can also be found in toes. So, a phalangeal fracture means you have broken one or more of the bones in your fingers or thumb. The most common way that a phalangeal fracture occurs is a direct blow. This could mean something has dropped on the hand, squished the hand, or the person has punched something.
In order to understand how these fractures occur, it’s important to understand what the phalanges are. The phalanges are actually the bones in your fingers, but they can also be found in toes. So, a phalangeal fracture means you have broken one or more of the bones in your fingers or thumb. The most common way that a phalangeal fracture occurs is a direct blow. This could mean something has dropped on the hand, squished the hand, or the person has punched something.
What Are the Signs and Symptoms?
 The common signs to watch for include not having full movement or flexibility of your fingers, pain, swelling, and loss of rotation, numbness, and severe bruising. A doctor will be able to take an x-ray and instantly see if there is a fracture. If you suspect you may have a broken finger, it’s best to have it looked at as soon as possible, so it can be properly set and treated.
The common signs to watch for include not having full movement or flexibility of your fingers, pain, swelling, and loss of rotation, numbness, and severe bruising. A doctor will be able to take an x-ray and instantly see if there is a fracture. If you suspect you may have a broken finger, it’s best to have it looked at as soon as possible, so it can be properly set and treated.
What Are the Common Treatments?
For a relatively minor fracture that doesn’t involve a number of bones, a simple splint and taping may be all that is necessary. Unfortunately, that isn’t the case for everyone and sometimes treatment can be more complicated. If the fracture was severe enough to damage the tissue and break through the skin, then you may need surgery to repair that area.
As well, depending on the bones that are affected, you may even need screws and pins put in place.
In very rare cases, there may be a total loss of motion for the finger that has been broken, and it’s always important to keep an eye out for infection. This is something your doctor will be able to watch for, and you will also need to be aware of the signs.
Schedule an appointment with the best plastic surgeon in Manhattan if you need surgery on your hand.
Contact us at 646-846-1136 to schedule an appointment.
Recovery Times and Side Effects from Gall Bladder Surgery
Many people who are due to have gall bladder surgery do not know what to expect when it comes to the side effects of this type of procedure or the recovery times required. Well, the first thing to remember is that this type of surgery can be carried out in one of two ways. Depending on the problem and a number of other factors, you may have to have open surgery for your gall bladder issue. Alternatively, you may be able to have the operation through keyhole surgery. The type of surgery you have will have an impact on the side effects as well as the recovery period.
Those that have keyhole surgery
If you are having a gall bladder operation through the use of keyhole surgery, the procedure will be far less invasive and involved. In fact, you should be able to go home on the day the procedure is carried out as long as there are no complications. In addition, the recovery period is much shorter than with open surgery. In general, you may be looking at around two weeks to recover from keyhole gall bladder surgery, after which time you can go back to your normal routine.
Those that have open surgery
The other alternative is open surgery, which is a far more involved procedure. When you have this type of surgery, you will be kept in hospital for a number of days before you are allowed to be discharged and go home. The recovery period following on from this type of open surgery is generally around six to eight weeks, so you will be out of action for some time before you can resume normal activities and routines.
Side effects of this type of procedure
You do not have to worry about long term effects of gall bladder surgery, as you can live a normal life without one. You will, however, experience some side effects from having this type of procedure carried out, although these are short term effects. Some of these include:
- Swelling, bruising, and tenderness around the wounds
- Nausea due to painkillers or anesthetic
- Stomach and shoulder pains
- Bloating and gas
- Diarrhea
- Low mood and feeling irritable
- Fatigue
Get in touch with a professional
If you have concerns about gall bladder surgery or you want to find out more information, you can get in touch with us today and speak to the best general surgeon in NYC.
Contact us at 646-846-1136 to schedule an appointment.
Possible Problems Stemming from Liver Surgery
 The liver is a vital organ in the body and it performs a number of crucial functions. This organ is responsible for making, breaking, and storing substances. It helps with all sorts of bodily functions such as digestion, blood clotting, and the storage of fat and glucose. This is just part of the functions that this vital organ provides, which is why it is important to keep your liver in the best condition possible.
The liver is a vital organ in the body and it performs a number of crucial functions. This organ is responsible for making, breaking, and storing substances. It helps with all sorts of bodily functions such as digestion, blood clotting, and the storage of fat and glucose. This is just part of the functions that this vital organ provides, which is why it is important to keep your liver in the best condition possible.
If you do have a medical problem that affects the liver, you may have to undergo liver surgery. The liver is an organ that we cannot live without so any conditions that have a major effect could result in the need for surgery. This can be major surgery and as with all major surgical procedures, it can come with risks. It is important to familiarize yourself with the possible risks so that you are fully prepared for your procedure.
Some of the main risks of liver surgery
 There are a number of potential risks and side effects that can stem from having liver surgery. Some of the ones that you should bear in mind if you are having this type of surgery include:
There are a number of potential risks and side effects that can stem from having liver surgery. Some of the ones that you should bear in mind if you are having this type of surgery include:
- Severe bleeding: Because of the amount of blood in the liver, an operation could result in heavy bleeding when the organ is cut. However, expert surgeons have the techniques and skills to minimize on this risk.
- Leakage of bile: Another risk during a liver operation is the possibility of bile leakage. The liver contains a number of bile ducts and the bile can leak from these once a cut has been made to the surface of the organ. This is a relatively rare occurrence and in most cases it sorts itself out without the need for additional treatment.
- Liver failure: If you have a section of the liver removed because of conditions such as cancer, the amount of the organ that is left behind may not be sufficient for your body. This could then lead to liver failure. This is one of the most serious possible problems connected to this type of surgery.
- Infections: As with many major surgical procedures, there is a risk of infection when you have liver surgery. This could include one of a range of infections or even multiple infections such as chest infections, abdominal infections, and infections of the wounds. In most cases, antibiotics are used to treat these.
Speak to the Best General Surgeon in NYC
Contact us at 646-846-1136 to schedule an appointment.
Colon Surgery for Cancer Patients
Colon cancer is a disease that affects many people, and there are a number of ways in which treatment is administered for this type of cancer. One of the most common treatments for colon cancer is surgery, particularly if the cancer is still in its very early stages. In this case, the colon surgery may be performed in order to remove the tumor, which may require part or the colon along with the lymph nodes to be removed. The latter is because the cancer will usually spread to the lymph nodes first, which is why they may be removed as part of the colon surgery.
The decision with regards to surgery and the type of surgery required will be based on a number of factors such as what stage the cancer is at, whereabouts it is located, and whether it has spread to other parts of the body. In addition, the surgeon will also need to take your age and general health into consideration when making a decision with regards to colon surgery. This procedure is performs by a specialist surgeon with expertise in bowel cancer and colon surgical procedures.
How is the operation performed?
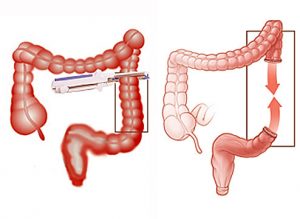 The process through which the surgery is performed will depend on a range of factors. When your doctor carries out tests to make a firm diagnoses, he or she will be far better placed to make a decision with regard to your treatment. In some cases, the procedure is carried out as open surgery, which means that you will have to prepare yourself for a lengthy recovery period following the procedure. However, in other cases it may be performed as keyhole surgery, which is less invasive and traumatic. It also means that you do not have to cope with such as long recovery period.
The process through which the surgery is performed will depend on a range of factors. When your doctor carries out tests to make a firm diagnoses, he or she will be far better placed to make a decision with regard to your treatment. In some cases, the procedure is carried out as open surgery, which means that you will have to prepare yourself for a lengthy recovery period following the procedure. However, in other cases it may be performed as keyhole surgery, which is less invasive and traumatic. It also means that you do not have to cope with such as long recovery period.
Additional surgery may also have to be carried out if the cancer has spread to other areas such as the liver or lungs. In these cases, chemotherapy is generally the treatment that is used to try and shrink and control the cancer. However, there may be cases where the surgeon decides upon surgery such as a liver or lung resection based on where the cancer has spread to. Again, this is something that the surgeon will decide upon and discuss with you following diagnosis and assessment.
Speak to one of the best general surgeons in NYC
 If you need advice about colon surgery and what is involved, you can get in touch with us and speak with one of the best general surgeons in New York City. Call us today and we will be happy to arrange an initial consultation
If you need advice about colon surgery and what is involved, you can get in touch with us and speak with one of the best general surgeons in New York City. Call us today and we will be happy to arrange an initial consultation
Contact us at 646-846-1136 to schedule an appointment.
Adrenal Gland Disorders: What are They?
The adrenal glands can be found at the top of the kidneys and their primary function is to deal with the release of various hormones. If these glands fail to generate enough of the hormone, or indeed if they produce too much, it can lead to problems. A number of different adrenal gland disorders can… Continue Reading
Surgical Treatments for Pancreatic Cancer
Pancreatic cancer is one of the most aggressive forms of cancer in humans and often the prognosis for patients is poor. There are several different types of pancreatic cancer and while many of them are often deadly, there is at least one type that is highly survivable. Because of the lethality of pancreatic cancer, most… Continue Reading
Common Types of Laparoscopic Surgery
Laparoscopic surgery is a type of minimally invasive surgery in which a number of small incisions are made, around a quarter inch in length each. Using smaller incisions means that patients experience less pain and a shorter recuperation period. Below is a guide to some of the most common types of laparoscopic surgery. Colon Laparoscopic… Continue Reading
What to Expect After a Liver Resection
A liver resection is a surgery to remove part of a patient’s liver. The liver is unique among all the interior organs in the human body in that it is capable of regenerating, meaning as much as 50 per cent of the liver can be removed during a resection; so long as the other half… Continue Reading
Recovering After a Splenectomy
A splenectomy is a surgical procedure where the spleen is removed. Most of you will have heard of a spleen, but surprisingly few people know where it is or what it does. The spleen is located under the left rib cage, near the stomach. It is a small organ, about the size of a human… Continue Reading
What to Expect from Laparoscopic Colon Resection Surgery
Colon surgeries account for more than 600,000 of the surgical procedures performed every year in the United States with colon surgery being used to treat a wide spectrum of diseases, including cancer, polyps, inflammatory bowel diseases; mainly Chron’s and ulcerative colitis. Colectomies or surgeries on the colon used to be invasive and have extensive recuperation… Continue Reading
What Is a Hernia?
Most of you will have at least heard of a hernia. In fact, a good percentage of you almost certainly know someone who has suffered from one, but you might not know exactly what one is, perhaps because a description of a hernia actually makes it sound far worse than it is. The good news… Continue Reading
Surgical Treatments for Pilonidal Cysts
A pilonidal cyst is a cyst located at the coccyx and they can present a problem if they become infected and pus filled. If this happens then it becomes a pilonidal abscess and these can be very painful. Initially, a pilonidal cyst looks like a pimple over the coccyx. They occur more in men than… Continue Reading
The Role of General Surgeons in The Hospital
Many people are familiar with the concept of surgeons having individual specialties. Generally, doctors and surgeons choose one area of the body to specialize in and, while a doctor in clinical practice will have to deal with multiple conditions affecting different parts of the body, surgeons rarely work outside of their preferred area. For this… Continue Reading
General Surgery
Here are some brief descriptions about the different types of general surgery we perform: Laparoscopic surgery This is a relatively new specialty dealing with minimal access techniques using cameras and small instruments inserted through 0.3 to 1 cm incisions. Robotic surgery is now evolving from this concept (see below). Gallbladders, appendices, and colons can all… Continue Reading